Legislature should pull plug on inept Medical Board of California

The time has come to put the Medical Board of California out of its misery.
The board oversees the licensing of doctors and their discipline for misdeeds or incompetence. It also has jurisdiction over doctor-owned surgical clinics. Long ago the board acquired the reputation of being one of the least effective regulatory bodies in Sacramento.
But evidence has mounted that it’s worse: It’s a danger to the community.
Because of its ineffectiveness in a variety of spheres, patients have died. Dangerous doctors have been allowed to continue operating for years after their malpractice first surfaced; surgical clinics allowed to remain open for years after dangerous conditions there were identified.
Today the board is facing a sort of medical crisis of its own: It’s up for legislative re-authorization under the state’s sunset rules. The legislators in charge of that procedure are talking about rubbing out the current membership and their executive director as of Jan. 1, and starting over fresh.
“That’s not an idle threat,” says Sen. Curren Price (D-Los Angeles), who chairs the board’s sunset review with Assemblyman Richard Gordon (D-Menlo Park).
Let’s hope not.
The board has sat inertly by while its disciplinary program against incompetent and dangerous doctors falls to pieces. Its regulation of the 1,200 physician-owned outpatient surgical centers under its jurisdiction — settings where patients routinely undergo surgery under potentially life-threatening conditions — is almost nonexistent.
“People are dying at these outpatient centers and your paramount responsibility is to keep that from happening,” Julie D’Angelo Fellmeth, a San Diego public interest lawyer who was appointed by the legislature to monitor the board’s enforcement program in 2003-2005, lectured the members last week. One would think the board knew that, but the news seemed to strike the members like a bolt from the blue.
The board’s enforcement record is dismal. Since 2007 California has typically ranked among the worst states in terms of serious disciplinary actions per 1,000 licensed physicians; the public interest group Public Citizen reported in 2011 that the board had failed to take action against more than 700 physicians whose privileges had been reduced or revoked by hospitals or other clinical settings, including 102 who had been found to pose an “immediate threat” to patients.
The board says statewide hiring freezes and furloughs have eroded its enforcement staff. But in 2010 it was given the authority to hire 18 investigators despite the freeze. It still hasn’t filled the positions.
The real crime of the medical board’s nonfeasance is that it’s a fraud on the public. Today’s board is largely the product of a major change in malpractice oversight in 1975. That’s when the legislature enacted MICRA, the Medical Injury Compensation Reform Act, to address a largely fabricated malpractice insurance “crisis.” MICRA limited payouts for malpractice judgments so severely that it effectively made malpractice lawsuits extinct in California.
In return for the elimination of patient lawsuits as a check on dangerous doctors, the medical profession agreed to accept tougher disciplinary standards and procedures from regulators. After a few more legislative tweaks, the medical board was born.
But the promise of tougher enforcement never was fulfilled. The legislature and governor’s office deserve plenty of blame for that. Although the board is funded entirely from license fees paid by doctors, not from taxpayer revenue, it wasn’t exempted from the layoffs and furloughs imposed by the Schwarzenegger administration as budget-cutting measures. Meanwhile, medical lobbies such as the California Medical Assn. have opposed efforts to increase license fees to adequately fund the board’s activities.
The board, which by law comprises eight physicians and seven “public” members, is unpaid except for expenses and per diems while on official business. (Four seats subject to appointment by Gov. Jerry Brown are currently vacant.) Californians get what they pay for: The members don’t seem to have any conception of the breadth of their authority, and precious little inclination to use it.
That was made evident by board President Sharon Levine’s appearance on March 11 before the sunset committee headed by Price and Gordon. Levine, an executive at Kaiser Permanente, made some remarkable assertions in her testimony. For example, she excused the board’s terrible record on discipline by explaining that it must wait for a complaint from a patient or other outside source before opening an investigation of a doctor.
In deference to Levine’s tenure on the medical board, which started in 2009 (she became president last year), I’m inclined to take a charitable view of this statement. So I’ll merely call it the single most ignorant description by a government regulator of his or her authority I’ve heard in 30 years.
The fact is that the board has all the power it needs to act on its own, with or without a complaint; indeed, such proactivity is the hallmark of effective state medical boards. In a blistering letter following the hearing, Price and Gordon cited the specific provision of California law that “unequivocally authorizes” the board to initiate its own investigations.
More blunders came when Levine addressed the board’s oversight of outpatient surgery centers owned by physicians, which came under its jurisdiction as the result of a state court ruling in 2007.
The board has outsourced oversight of these clinics, which perform an increasing number of such serious procedures as weight-loss and cosmetic surgeries, to four private, nonprofit accreditation organizations. These accreditors are not government regulators. They don’t have subpoena power or the authority to close down a dangerous clinic, and they don’t have consistent standards or procedures for granting accreditation.
The accreditors are paid by the surgical centers to issue their seals of approval, a flagrant conflict of interest that gives the accreditors a financial incentive to go easy. For a time, centers that lost accreditation from one of the four often could simply acquire approval from another, no questions asked. After I exposed the practice in a series of columns in 2010 and 2011, legislation by Price ended that sort of bed-hopping.
Price’s measure required the board to collect information about every one of those centers, including the identity of their physician owners and their accreditation histories. The data were to be posted on a website so consumers can know exactly who they’re dealing with when they go to these non-hospital settings for operations. Yet according to a study by Consumers Union, two-thirds of the listings still don’t identify a doctor-owner; 30% of the listings don’t provide the required accreditation records.
The board has yet to take its oversight of surgical centers seriously. “We don’t regulate the [surgical] settings,” Levine told Price and Gordon. “All we can do is regulate the agencies that accredit.”
This is also 100% wrong. Here’s what the law says: The Medical Board “may enter and inspect any outpatient setting ... at any reasonable time to ensure compliance with, or investigate any alleged violation of,” the California health and safety law. If the inspectors don’t like what they see, they can ask the attorney general or a local district attorney to act to shut down the place.
Most amazingly, Levine told the lawmakers that her board’s members “have a keen interest in understanding the process of accreditation and in learning what the differences are among the four (organizations) in terms of their process, procedures and criteria for accreditation.” Accordingly, they invited all four to make presentations on these topics last week.
Wrap your mind around this: The medical board has had legal authority over the accreditation process since 1996. It has been relying on these organizations for its regulation of outpatient centers performing major surgery since 2007 — six years ago. And they just got around to inquiring how accreditation works last Thursday?
It was after Levine’s appalling performance in March that Price and Gordon raised the prospect of letting the sun set on the current board and its executive director, Linda Whitney. If that were to happen, they would be tossed out of their jobs Jan. 1 to make way for newly appointed individuals. State laws governing licensing and discipline would remain in effect and the board’s staff would remain employed.
Not everyone thinks the change would be ideal. Fellmeth observes that the risk of sunsetting is that it will put inexperienced people in place — it might be better to leave the somewhat experienced people on the board “and push them to do better.”
The most effective change, she says, would be to move all of the board’s investigators over to the attorney general’s office to provide consistent enforcement. That’s an idea that has been under consideration since 2005, and just last week was added to a regulatory reform bill sponsored by Price. The board opposes the change.
But a drastic overhaul plainly is needed. All healthcare stakeholders are harmed by a do-nothing and know-nothing board. Good doctors should be incensed that the board allows bad doctors to continue practicing, sullying the reputation of the entire profession. Bad medicine drives up costs for insurers, who pass them on to their customers. And patients are more at risk of physician-caused injury and death.
This board has been comatose so long it’s beyond resuscitation. Pull the sheet over its eyes and notify next of kin. The idea of sunsetting the board and starting over is the right one. The only question Californians should be asking is: Do we really have to wait until January?
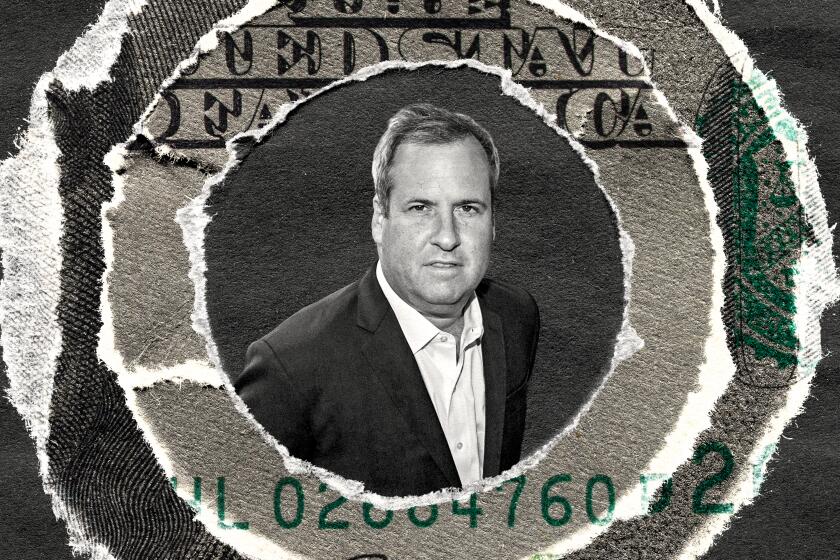
Michael Hiltzik’s column appears Sundays and Wednesdays. Reach him at [email protected], read past columns at latimes.com/hiltzik, check out facebook.com/hiltzik and follow @latimeshiltzik on Twitter.
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production — and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.