Coronavirus testing is under scrutiny after delays and questions over its effectiveness
The four-day delay in testing a Northern California patient who appears to be the first in the United States to contract the coronavirus from community contact highlights growing questions about the federal government’s testing policies and protocols as the virus continues to spread.
A growing number of experts have said problems with the test process — including ineffective test kits and restrictive rules on who gets tested — could be fueling the undetected spread of the virus.
“When you miss cases, you can’t isolate them, test their families or get a hold on this before it keeps spreading,” said Jennifer Nuzzo, an epidemiology expert at the Johns Hopkins Center for Health Security.
Until Thursday, the Centers for Disease Control and Prevention restricted coronavirus testing to patients with clear symptoms of infection who have either traveled to China recently or who have been in contact with someone who has tested positive for the virus. As the virus outpaced detection efforts around the world, that gateway to testing proved far too narrow.
As early as last week, doctors at the UC Davis Medical Center suspected a coronavirus case and immediately requested testing from the CDC. But it was another four days before the test was done. During that time, others in the area could have been exposed to the virus.
On Thursday, the CDC expanded the criteria for who qualified for testing to include sick patients who had traveled to Iran, Italy, Japan and South Korea. They will also test severely ill patients with acute lower respiratory sickness who are hospitalized, even those who have no known link to the coronavirus outbreak.
The CDC faces growing political backlash.
California Sen. Dianne Feinstein on Thursday called on the White House to start rapid testing of all suspected cases, saying the identification of coronavirus patients quickly is essential to limiting the spread.
Gov. Gavin Newsom said California is in desperate need of test kits. The state has 200 kits for both diagnostic and surveillance purposes, but federal officials say more will arrive in the coming days, he said.
“We are currently in deep partnership with the CDC on one overriding protocol that drives our principal focus right now, and that’s testing,” Newsom said, calling expanded testing “our top priority, not just in the state of California but, I imagine, across the United States.”
Such an expansion includes both broadening the criteria that a person must meet to be tested for COVID-19, as well as getting more coronavirus test kits sent to California, he said.
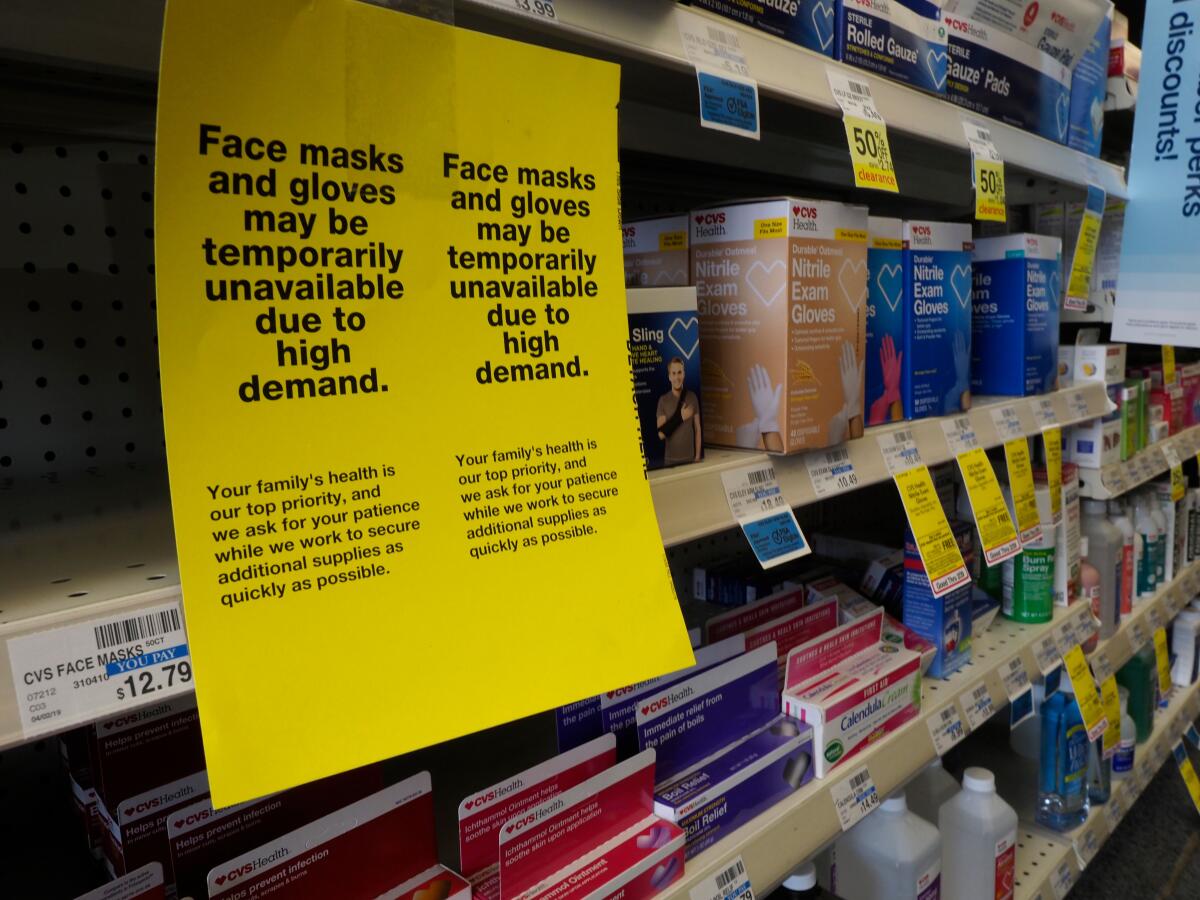
The kits have come under growing scrutiny.
The CDC distributed the test kits to partner laboratories across the country, but many of those campuses ran into problems with one of the ingredients, leading to inconclusive test results. Most public health officials needed to send specimens to the CDC’s central laboratories in Atlanta for testing, a process that can take up to 48 hours, creating a bottleneck.
“We’ve only had a handful of labs that can test with it. The rest have been on pause,” said Scott Becker, the executive director of the Assn. of Public Health Laboratories. “When you’re waiting 48 hours to get a response from the CDC, you’re burning through equipment caring for a patient, just waiting to see the results.”
The problem grew so troublesome that state and local laboratories began seeking permission from the Food and Drug Administration to bypass standard regulations and design and launch their own tests, rather than rely on the federal one.
On Thursday morning, Health and Human Services Secretary Alex Azar told members of Congress that the problem had been resolved. The FDA approved a modified protocol that circumvents the issue.
Forty local and state public health labs, as well as some labs run by the Pentagon, are already authorized to begin using the modified test, and more than 50 others will be doing the same by next week, he added.
Delays and missteps in coronavirus testing have caused major issues across the country, where public health officials on the front lines are stretched thin. Epidemic preparedness is already “a victim of roller coaster funding,” Becker said, and the baseline shortages of equipment and personnel are exacerbated.
In addition to preparedness duties — developing local guidance, tracing patients’ contacts, working with schools and churches to the community — officials are having to do more for people quarantined at home. Health workers are delivering groceries to keep them at home, said Adriane Casalotti, the chief of government and public affairs at the National Assn. of County and City Health Officials.
Above all, the burden on individual families is heaviest.
“In most jobs in this country, you can’t work from a laptop on your couch. When there are delays in diagnostics, we’re out there asking real people to choose between the public’s health and their own financial well-being — them keeping their jobs. For individual families, this is complicated and messy,” Casalotti said.
Once the coronavirus begins to spread, even those who aren’t infected will have to deal with school closures, telecommuting and other adjustments.
Critics said the slow testing process could mean coronavirus is already spreading in U.S. communities. But because the virus’ symptoms are frequently mild, people might be spreading it unknowingly.
A Japanese couple visiting Waikiki Beach in Hawaii tested positive for the virus after returning to Asia, but Nuzzo and other epidemiologists say the virus’ incubation period hints that they could have contracted it on U.S. soil.
Hawaiian authorities were so alarmed by the limited testing capabilities in the U.S. that they requested permission from CDC authorities to use a tool from Japan.
On Thursday, the focus around coronavirus in the U.S. centered on Solano County.
UC Davis officials said the coronavirus patient arrived at its medical center from another hospital Feb. 19 but was not tested until Sunday. There is no evidence the woman had traveled from a coronavirus hotspot or was in contact with someone who had. The hospital said that precautions had been put in place because of healthcare workers’ concerns about the patient’s condition. It asked a “small number” of employees to stay home and monitor their temperature.
The woman was “in her community” for a number of days before accessing care, California Health and Human Services Agency Secretary Dr. Mark Ghaly said Thursday.
Investigators are now working to find and contact any people who may have come in contact with the woman. The CDC has sent 10 staffers to help trace her contacts, Newsom said.
Healthcare workers, including some students from UC Davis and other colleges, are under self-quarantine because they might have been exposed to the virus.
Solano County is also home to Travis Air Force Base, where several hundred people were quarantined after returning on repatriation flights from Wuhan, China, and the Diamond Princess cruise ship in Japan. A whistleblower complaint on Thursday alleged that federal health workers were not provided adequate training and protective gear when dealing with quarantined people at Travis and a second California base.
A total of 33 people have been diagnosed with coronavirus in California, and five have since left the state, Newsom said. Of the confirmed cases, 24 were either evacuated from the Diamond Princess cruise ship or returned on repatriation flights from Wuhan, the epicenter of the coronavirus outbreak.
Newsom said more than 8,400 people are being monitored in 49 local jurisdictions.
COVID-19 has infected more than 80,000 people in about three dozen countries since it was discovered in late December. More than 2,700 have died, most of them in mainland China.
There are currently 60 confirmed cases in the United States.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.