Your guide to the latest in cancer screening tests: Which do you need, which can you skip?
Cancer screening could save your life. Then again, it could give you a false alarm or lull you into a false sense of security.
Screening is a science, but it’s not an exact science.
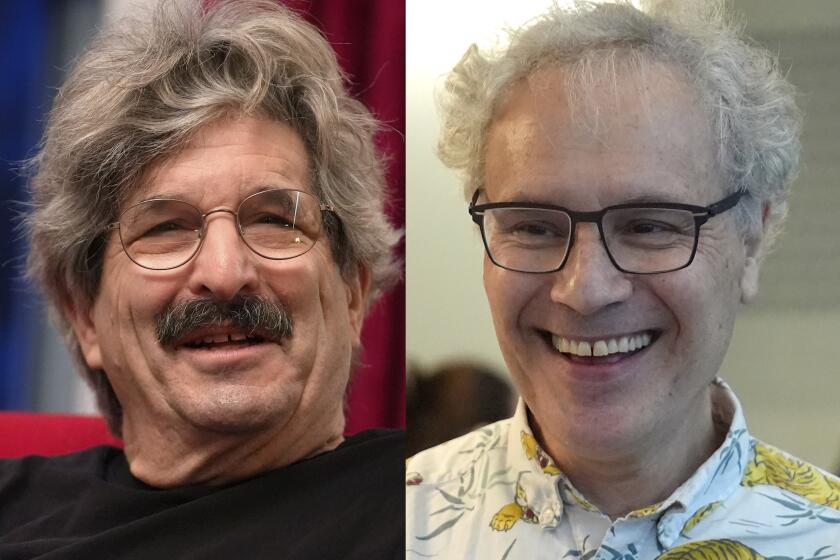
“Sometimes people think it’s better than it actually is,” says Dr. Otis Brawley, chief medical officer for the American Cancer Society.
But just because screening isn’t perfect doesn’t mean it’s not useful. At its best, it functions as an early-warning system, finding signs of trouble before you have any symptoms. That gives you a jump on cancer — and the option of starting treatment early, when it may well be more effective.
Still, Brawley cautions, it’s wise to keep in mind that a screening test can’t guarantee that you’re cancer-free, even if it doesn’t find anything wrong. Nor does a troubling result necessarily mean you have cancer — it’s just a warning that you should have more tests.
Doctors use different methods to screen for different kinds of cancers. Tests vary widely in terms of accuracy, safety and usefulness.
Fortunately, a number of government agencies, expert panels and medical organizations keep close tabs on the latest research and offer professional guidance about who should be screened for what, and how often. All these groups emphasize the importance of discussing your own situation with your healthcare provider.
Breast Cancer
The American Cancer Society recommends a screening mammogram every year for women between the ages of 45 and 54, then every other year from ages 55 and up. Screening should continue as long as women are in good health and expect to live at least 10 more years.
The U.S. Preventive Services Task Force advises women to receive a screening mammogram every other year between the ages of 50 and 74.
Both groups say women should understand the known benefits, limitations and possible harms associated with breast cancer screening. They also say that screening could begin as early as 40 if women are informed about the pros and cons of doing so.

The American Cancer Society says women may be screened annually if they prefer. But the task force warns that yearly tests are more likely to lead to unnecessary treatment than to saving lives.
Some women may need to be screened with MRIs as well as mammograms, but this is appropriate only for a very small number of people. A healthcare provider can help determine who belongs in this group.
The
Colorectal cancer and polyps
Both men and women should begin screening at age 50, according to the American Cancer Society.
To test for both cancer and polyps requires a colonoscopy every 10 years (preferred) or a less invasive test every five years. These include a CT colonography (a.k.a. virtual colonoscopy), a flexible sigmoidoscopy, or a double-contrast barium enema. If any of these test results are positive, a follow-up colonoscopy is necessary.
It’s possible to screen for cancer, but not necessarily polyps, with a fecal immunochemical test (FIT) or a guaiac-based fecal occult blood test once a year. These tests use a multiple stool take-home test. A third option is to take a stool DNA test (sDNA) every three years. If any of these test results are positive, they should be followed up with a colonoscopy.

Doctors say it’s better to screen for both cancer and polyps. But if those tests aren’t available, or are too off-putting, select an option from the second group instead. What matters most is getting tested.
Those at high risk for colon cancer may need to follow a different schedule. Patients should discuss their individual risk with their healthcare provider.
The U.S. Preventive Services Task Force recommends screening between the ages of 50 and 75. After that, options should be discussed with a doctor. The task force does not recommend any single “best test” for everyone. With the help of a doctor, patients should pick a test based on their preferences, medical condition, how willing they are to have the test, and what tests and follow-up procedures are available.
Cervical cancer
Screening with a Pap test should begin at age 21 and continue every three years until age 29, according to the American Cancer Society, the U.S. Preventive Services Task Force and the American Congress of Obstetricians and Gynecologists. An HPV test is not recommended unless indicated by an abnormal Pap test.
The ACS and ACOG both say that between ages 30 and 65, it’s best for women to have a Pap test along with an HPV test every five years, although having only a Pap test every three years is an acceptable alternative.
Those who have been vaccinated against HPV still need to follow the screening recommendations.
After age 65, women who have been tested regularly with normal results for the past 10 years should stop being screened, the ACS says. Once screening has stopped, it should not start again.

Women who have been diagnosed with a serious cervical pre-cancer should keep being tested for at least another 20 years, even if that means being tested after age 65.
Women should not get tested if they’ve had their uterus and cervix removed for reasons unrelated to cervical cancer and their pre-surgery screenings never showed signs of cervical cancer or serious pre-cancer.
Patients should discuss their personal health history wth their healthcare provider. Things like HIV infection and exposure to diethylstilbestrol (prescribed to prevent miscarriages) may affect the screening schedule.
The Centers for Disease Control and Prevention call the Pap test one of the most reliable and effective cancer screening tests available. The CDC website summarizes guidelines from a number of other respected agencies and organizations here.
Endometrial (uterine) cancer
Screening is not recommended, but women should discuss the risks and symptoms of endometrial cancer with their healthcare provider at menopause. A yearly endometrial biopsy may be warranted in some cases, depending on the patient’s personal health history.
Any unexpected vaginal bleeding or spotting should always be reported.
Lung cancer
Screening is considered only for those who have smoked a minimum of a pack of cigarettes a day for 30 years, or the equivalent (for instance, three packs a day for 10 years).
Men and women between the ages of 55 and 74 who still smoke or who have quit only within the last 15 years should talk to their healthcare provider about whether screening is right for them, according to the the American Lung Assn., the American College of Chest Physicians and the American Society of Clinical Oncology.

The American Cancer Society adds that people should be screened only if they are in good health. The U.S. Preventive Services Task Force advises people to consider screening up through the age of 80.
Those who decide to be screened should get a low-dose CT scan once a year.
The Centers for Disease Control and Prevention summarize the advice from a number of organizations here.
Prostate cancer
There is no proof that the possible benefits of screening for prostate cancer outweigh the possible harms, including the risk of suffering side effects from unnecessary treatment. Starting at age 50, men should discuss these issues with a healthcare provider, and they should not be tested until they are fully informed, the American Cancer Society says.

African American men and men with a father or brother who had prostate cancer before age 65 should have this discussion at age 45.
Those who decide to be tested should have a PSA blood test with or without a rectal exam. The PSA level will determine how often they should be tested in the future, as well as what kind of test to have.
The Centers for Disease Control and Prevention, in accordance with the U.S. Preventive Services Task Force, recommend against PSA screening for men who do not have prostate cancer symptoms.
Skin cancer
The American Cancer Society makes no recommendations about screening for any type of

The U.S. Preventive Services Task Force has concluded that there is not enough evidence to recommend for or against screening for those who don’t have a history of skin cancer and do not have any questionable moles or other spots.
The Skin Cancer Foundation recommends that people check their own skin once a month. It also advises an annual head-to-toe skin exam from a doctor to screen for melanoma, the most dangerous type of skin cancer.
Thyroid cancer
The U.S. Preventive Services Task Force recommends against screening for adults who have no symptoms. The American Cancer Society makes no recommendations about thyroid cancer screening.
Ovarian cancer
The American Cancer Society makes no recommendations about ovarian cancer screening. The U.S. Preventive Services Task Force advises against screening for healthy women with no genetic mutations that would raise their risk for the disease.
The Centers for Disease Control and Prevention have found no evidence that any screening test reduces deaths from ovarian cancer.
MORE IN HEALTHY LIVING
With cancer, it's not necessarily where it starts but how it starts
When it comes to cancer, here's what you should sweat and here's what you shouldn’t
Curing cancer isn't always the goal. Sometimes you just want it to be a manageable chronic disease