Op-Ed: How rising hospital costs increase healthcare inequities for marginalized communities

Across the state, California’s hospitals are facing serious challenges — particularly those institutions serving our urban, low-income and historically marginalized communities. Metropolitan anchor hospitals, as they have come to be known, play a vital role in advancing health equity and are disproportionately affected by the problems facing the entire healthcare system.
Healthcare costs, which were already increasing before the COVID-19 pandemic, are now accelerating at an even faster pace. Inflation, supply chain issues and rising labor costs are making the situation even more dire. Today’s economic headwinds have tremendous implications for the metropolitan anchor hospitals and their ability to improve patient access to care, reduce healthcare disparities and advance equity in some of California’s most economically challenged neighborhoods.
The trends here mirror what is happening nationally. In 2020, healthcare costs represented nearly 20% of the United States’ gross domestic product, a sharp rise from 2019 and more than four times higher than in 1960. COVID-19 helped fuel the rapid acceleration of healthcare costs, pushing hospitals to the brink. For America’s urban safety net hospitals, these increases have made it even harder to provide care in high-need communities.
Too few doctors can afford to practice in the communities that rely on Medi-Cal, which are largely made up of people of color.
Labor costs have been particularly challenging, driven by soaring demand for care throughout the pandemic while many hospitals and health systems were also experiencing critical shortages of physicians, nurses and other essential staff. To fill the void, many hospitals were forced to rely on staffing agencies. Hourly rates of contract staffing agencies increased by 213% from pre-pandemic levels in January 2019 to this year, according to a recent American Hospital Assn. report. This put even more financial strain on the metropolitan anchors, which often operate with far fewer resources than other hospitals, even those serving the same areas.
On average, a hospital spends approximately half of its budget on its workforce. So, when per-patient labor expenses rose by nearly 20% from 2019 to 2021, many hospitals — especially metropolitan anchors, which treat high numbers of Medicare and Medicaid beneficiaries and provide high levels of uncompensated care — found themselves in a bind. Credit rating agency Fitch recently adjusted its outlook for the not-for-profit hospital sector, forecasting that “labor expenses may be reset at a permanently higher level for the rest of 2022 and likely well beyond.”
With researchers predicting a shortage of up to 3.2 million healthcare workers by 2026, the crisis is expected to get much worse. By the end of this year, estimates suggest the U.S. may experience a shortage of as many as 1.1 million nurses, a problem that will only be compounded by many physicians and other health professionals also leaving the field.
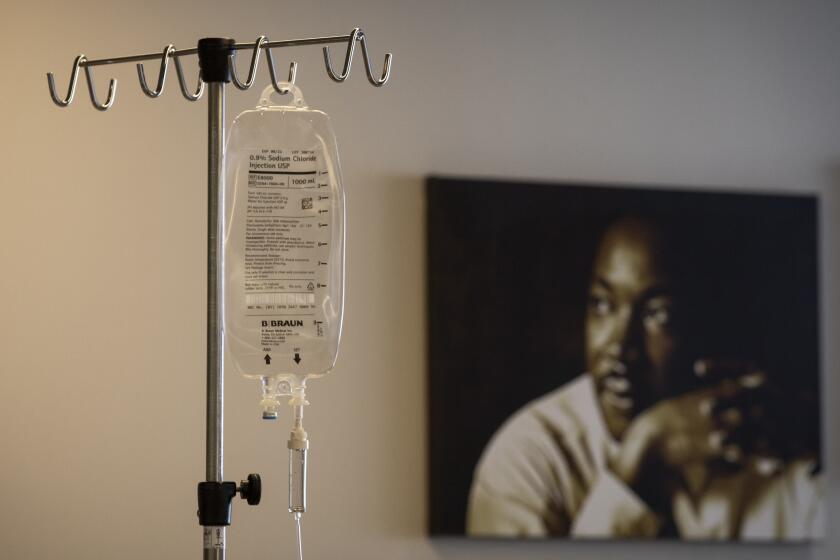
Hospitals’ financial instability is compounded by supply chain challenges, inflating the costs of drugs, supplies and medical devices. For example, data show that per-patient drug expenses increased by nearly 40%, and per-patient supply costs rose by approximately 20% in 2021. These trends are simply unsustainable.
These escalating healthcare costs can have dire consequences for health equity. Metropolitan anchor hospitals typically have razor-thin or negative margins, which hinders their ability to weather financial storms. I fear these hospitals will be forced to make tough decisions about their ability to provide the same level of high-quality care that every individual deserves. If these hospitals are not given federal government support to stay afloat, they will find it even more difficult to attract and retain staff, modernize their facilities and continue offering programs that address the social factors that influence health.
The people likely to suffer most from new cuts to COVID relief programs are communities of color, especially Latinos.
Hospitals, especially established institutions in large urban or metropolitan areas, are vital to reducing health disparities. Here in Los Angeles, hospitals such as Martin Luther King Jr. Community Hospital and East Los Angeles Doctors Hospital are pillars of marginalized communities. Throughout California and the country, many anchor hospitals operate primary care and specialty clinics in high-need neighborhoods, participate in public-private partnerships to provide affordable housing to residents, manage community gardens and “food pharmacies,” and coordinate anti-violence programs. These initiatives are part of an overall strategy to improve health outcomes and enhance the quality of life for patients in need.
I’m still optimistic that the greater focus on improving outcomes for patients in marginalized communities will go a long way toward ending the shameful health disparities that exist. Stakeholders throughout the healthcare sector are working to develop a legislative proposal that would establish a federal designation distinguishing metropolitan anchor hospitals, helping to ensure they have adequate resources to continue providing high quality care. It would be similar to the way critical access hospitals are designated in rural areas.
We need Congress to recognize the unique services delivered by, populations served by and financial barriers faced by metropolitan anchors, and to create this type of designation to help communities that depend on these institutions.
Governments — federal, state and local — must provide the resources to ensure that these vital hospitals are not struggling to survive, but instead thriving and continuing the mission of health equity.
Julianne Malveaux is an economist, author and dean of the College of Ethnic Studies at Cal State Los Angeles.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.