Soaring insurance deductibles and high drug prices hit sick Americans with a ‘double whammy’

Wendy Matney hesitated to tell her family not to call 911.
“It seemed almost selfish to say, ‘Please don’t call because we can’t afford this,’” said the 39-year-old home health aide, who has a form of epilepsy that causes frequent, sometimes violent, seizures.
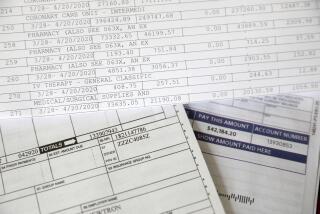
Matney has been to the hospital enough, though, to know a trip means thousands of dollars in bills under the family’s high-deductible health plan. And she and her husband — struggling with more than $20,000 in medical debt — can afford no more.
Hit with a hospital lawsuit over unpaid bills, the couple are declaring bankruptcy, effectively giving up hope of moving out of their trailer and buying a house.
“I’m losing everything because of this,” Matney said.
The steep rise in health insurance deductibles over the last decade has saddled insured, middle- and working-class Americans with medical bills they can’t afford, a Los Angeles Times examination of job-based insurance shows.
Health insurance deductibles soar, leaving Americans with unaffordable bills »
The biggest impact, however, has been on people like Matney who have illnesses such as diabetes, cancer and epilepsy that require regular medications and consistent care.
As drug prices have skyrocketed and deductibles in job-based coverage have more than tripled in the last 12 years, soaring to an annual average of $1,350, these sick Americans now routinely pay thousands of dollars every year to get care they need. That has made being sick in the U.S. dramatically more expensive.
“It’s really a double whammy,” said Dr. Brian Callaghan, a University of Michigan neurologist who has studied the impact on people with neurological illnesses.
The financial strain is pushing millions of seriously ill Americans to ration their care, jeopardizing their health and even their lives.
In 2016, for example, Americans taking multiple sclerosis medications every month paid on average $3,708 a year out of pocket for the drugs. Patients in high-deductible health plans paid even more, with average annual costs of nearly $8,000, according to a study by Callaghan.
Fifteen years earlier, the out-of-pocket costs for those medications were $244 on average, adjusted for inflation.
The average patient with lymphoma, a common blood cancer, pays nearly $3,700 in the 12 months following the diagnosis, according to an analysis of commercial insurance data by Milliman, a national healthcare consulting firm. Patients with acute leukemia pay more than $5,100.
Most patients now diagnosed with cancer don’t understand how severe the financial strain will be, said Dr. Scott Ramsey, director of the Hutchinson Institute for Cancer Outcomes Research in Seattle.
Analyzing bankruptcy records and cancer registries in Washington state, Ramsey found that cancer patients were more than 2½ times more likely to declare bankruptcy than people without the disease, even after accounting for differences in age, socioeconomic status and other factors.
“Suddenly, people find they owe hundreds or thousands of dollars,” Ramsey said. “If they are young or working in a low-wage job, they’re not going to be able to pay.”
Several Western European countries, including Britain and France, which have national healthcare systems, limit cost sharing for people with some chronic conditions, making prescription drugs available at no cost to patients.
Holland, which relies on private insurance, requires insurers to exempt primary-care visits from any cost sharing.
In the U.S., however, federal law generally prohibits high-deductible plans from exempting these services, forcing patients to pay for them in full until they meet their deductibles.
“What we’re doing makes no sense,” said David Grabowski, a health policy researcher at Harvard Medical School.
Grabowski’s work has shown that epilepsy patients like Matney who have high out-of-pocket medical costs were less likely to fill their prescriptions and more likely to end up in an emergency room or to be admitted to a hospital, leading to higher costs.
“We want these people to take their medications. That’s not only good for their health, it’s good for overall healthcare spending,” he said. “This is penny wise and pound foolish.”
Across the country, organizations that work with sick patients increasingly report being called upon to aid people who cannot afford care, despite having insurance.
“High-deductible health insurance may be OK for patients with means who can manage their expenses,” said Lisa Lacasse, president of the advocacy arm of the American Cancer Society. “For the majority of people diagnosed with cancer, they are deeply problematic.”
Susan Brown, who oversees the patient support program at Susan G. Komen, said most people who call the breast cancer group are seeking financial assistance.
“The stories we hear are heartbreaking,” she said. “People cashing in their college funds, taking on a second mortgage, maxing out their credit cards.”
Americans in a household where someone has a serious medical condition are twice as likely as healthier Americans to say they’ve cut spending on food, clothing and other household items to pay for care, according to a nationwide poll of people with job-based coverage conducted by The Times in partnership with the nonprofit Kaiser Family Foundation, or KFF.
One in eight covered workers in a household where someone is chronically ill reported having declared bankruptcy because of medical bills.
How the L.A. Times/Kaiser Family Foundation poll was done »

Matney, who lives in an aging mobile home in a mountainous corner of northeastern Tennessee, had her first seizure in her mid-20s. She qualified for Medicaid while her children were young and unpredictable seizures made holding a job difficult.
The subsidized government coverage allowed Matney to get recommended medications and tests, see a neurologist and enroll in cognitive therapy.
The treatment regime didn’t cure her — medication fails to control seizures in about a third of epileptic patients — but Matney didn’t have to fear catastrophic medical bills.
“It was good coverage,” she said.
In 2013, she met Steve Matney while playing an online Facebook video game.

He’d worked for a dozen years at a Walmart distribution center, where he earned about $33,000 a year, budgeted carefully and avoided debt. Five years older than Wendy, Steve owned a trailer home and took care of his aging mother, who lived next door.
“He had such a sweet, caring nature,” Wendy remembered. “He was very much his own person … but at the same time, he was so supportive.”
The couple married in 2014.
Wendy didn’t realize that marrying and moving onto her new husband’s job-based insurance could prove financially ruinous for both of them.
Just a few months after the wedding, she had a major seizure — convulsing on the bathroom floor and struggling for breath. Fearing for Wendy’s life as her lips turned blue, Steve called 911.
An ambulance took her to a community hospital, where doctors ran tests and kept her overnight for observation.
The bills ran to thousands of dollars.
“It was definitely a shock,” Wendy said. “I guess I hadn’t realized how much it all cost.”

Are you facing high medical costs because of a high-deductible health plan? Tell us your story »
There would soon be more bills. Matney estimates she’s been to the emergency room several dozen times in the last five years, almost always after she lost consciousness and someone called an ambulance. The couple, whose deductible is now $5,500, pay what they can, she said. But the bills almost always go to collections.
Wendy has pleaded with her family not to call an ambulance and to wait for her seizures to pass. She’s tried to convince emergency room staff not to admit her to the hospital. She’s rarely been successful, though.
Last year, Ballad Health, a nonprofit that owns the local hospital, sued the Matneys over more than $11,000 in unpaid bills. After securing a court order, Ballad began garnishing a quarter of Steve’s salary, leaving him $663 every two weeks.
“That’s been hard,” Wendy said.
High costs increasingly push patients like Matney to skip care, physicians and researchers find.
At the Duke Cancer Institute in North Carolina, Dr. S. Yousuf Zafar said oncologists frequently see patients who have insurance but don’t follow through on therapy for fear of the costs.
“There are drugs that we know work,” he said. “But patients aren’t taking them.”
Zafar recalled a man with pancreatic cancer who elected to stop treatment. “He said, ‘I’d rather not have this chemotherapy because I don’t want to leave my family with tens of thousands of dollars in medical bills.’”
Dr. Ana Maria Lopez, an oncologist at the Sidney Kimmel Cancer Center in Philadelphia, said one of her breast cancer patients put off chemotherapy and radiation treatment for two years. “She had promised herself she would get her daughter through high school,” Lopez said.
Half of all Americans in a job-based health plan say they or an immediate family member have delayed a doctor’s appointment, not filled a prescription or postponed some other medical care in the last year because of cost, The Times/KFF survey found.
Among people with a serious medical condition, that share rises to 6 in 10. Among covered workers in plans with at least a $3,000 individual or $5,000 family deductible, it’s three-quarters.
New research conducted in partnership with The Times for this project also shows that sick Americans use less healthcare when their plan requires them to pay more out of pocket.
Analyzing data from about 10 million people with commercial insurance, the Health Care Cost Institute — a Washington-based think tank — found that in 2016, patients with Type 2 diabetes who were in a high-deductible plan filled fewer prescriptions and saw a physician less often than those in plans with lower cost sharing.
The institute found similar patterns among people with hypertension and Chronic Obstructive Pulmonary Disease, or COPD.
“Across the board, people in high-deductible plans are using less care,” said William Johnson, the report’s lead author. “When you shift costs onto patients, they respond…. It’s a very powerful incentive.”
Tracking patients for many years to figure out how rationing affects health is difficult. But researchers are beginning to find signs of a toll.
In one recent study, low-income workers and their family members with diabetes sought nearly 22% more emergency care for avoidable complications after they switched to a high-deductible plan.
“People with very high incomes can probably absorb the higher cost sharing,” said Dr. J. Frank Wharam of Harvard Medical School, the study’s lead author. “Unfortunately, it’s lower-income people in these plans who are suffering worse outcomes.… It’s clear some are being hurt.”
Other research indicates that the financial strains may shorten patients’ lives.
In addition to discovering higher bankruptcy rates among cancer patients, Ramsey, the Washington researcher, found that people with certain common cancers who did go bankrupt died sooner than similar cancer patients who did not.
Matney, whose coverage on her husband’s health plan means she no longer has the financial protections provided by Medicaid, said she now frequently rations care to save money.
Although neurologists typically recommend that epileptic patients with uncontrolled seizures experiment with drugs to find which work best, Matney sticks with low-cost generics.
Last year, she got into a prescription assistance program that allowed her to take a more costly brand-name drug. It seemed to work better, but she had to stop when she could no longer get the medication for free.
She also stopped seeing a neurologist or getting regular blood tests, which are recommended to ensure patients taking epilepsy drugs are getting the right doses.
“I still owe them from last year,” she said, “and we can’t pay right now.”

Matney is trying to make ends meet by taking on extra work as a home health aide. She recently got a job with the agency that provides assistance to her 67-year-old mother-in-law, which allows Matney to walk to work. She gets paid $9 an hour.
She is trying a new diet and using cannabis oil, hoping that may control her seizures. Sometimes, she puzzles over why health insurance costs so much for people like her.
“I guess I understand why they do it,” she said. “But there is absolutely no help for people who have to go to the doctor because they’re sick.… I’m being charged an incredible amount of money just to live. It somehow doesn’t feel fair.”
More stories from Noam N. Levey »
More to Read
Get the L.A. Times Politics newsletter
Deeply reported insights into legislation, politics and policy from Sacramento, Washington and beyond. In your inbox three times per week.
You may occasionally receive promotional content from the Los Angeles Times.