Coronavirus Today: The payoff of mask mandates
Good evening. I’m Karen Kaplan, and it’s Friday, Aug. 13. Here’s the latest on what’s happening with the coronavirus in California and beyond.
You can grumble about the fact that even fully vaccinated people are being asked — and in some cases required — to wear masks indoors again as the Delta variant runs amok across California. But it’s getting harder to deny that those masks are making a difference.
Experts are pointing to indoor mask mandates like the one in Los Angeles County as a major reason why the Golden State has managed to avoid the sky-high coronavirus infection rates and increasingly overcrowded hospitals seen in other parts of the country.
Our better-than-average vaccination rates have offered protection too. More than 63% of Californians have received at least one dose of COVID-19 vaccine, and 54.7% are fully vaccinated, according to our vaccine tracker. Nationwide, 59.2% of Americans are at least partially vaccinated and 50.4% are fully vaccinated, the Centers for Disease Control and Prevention report.
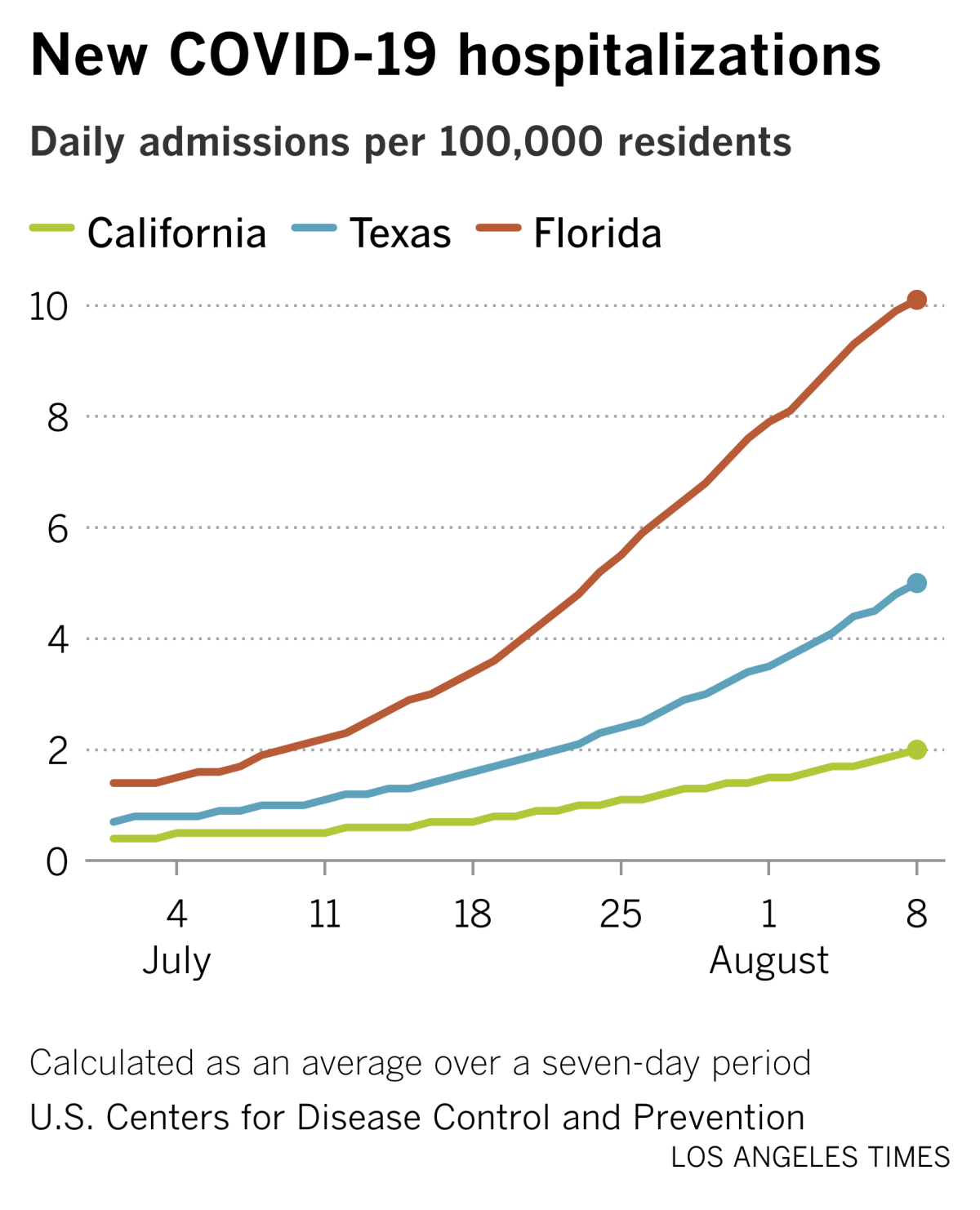
But mask policies are interesting because there’s such a clear difference between California’s approach and those of Texas and Florida, which rank right behind us in terms of population.
It’s been a little more than two weeks since state health officials recommended that fully vaccinated people resume wearing masks in indoor public settings. L.A. County’s universal indoor mask mandate is nearly a month old, and it’s been copied by other counties, including Santa Barbara, Sacramento and much of the San Francisco Bay Area.
Texas Gov. Greg Abbott and Florida Gov. Ron DeSantis, on the other hand, are not only opposed to statewide mask mandates, they don’t want local governments in their states to implement them for themselves.
(You may recall that DeSantis threatened to have his state’s Board of Education withhold the salary of a school superintendent in Tallahassee if he imposed a mask mandate for students. Nonetheless, some school districts in Florida are proceeding with them, as are several in Texas.)
My colleagues Rong-Gong Lin II and Luke Money looked into how those differing approaches are playing out in terms of each state’s COVID-19 caseload. The differences they found are striking.
Over a seven-day period that ended this week, California reported 141.1 new coronavirus cases per 100,000 residents. That’s less than half the rate for Texas, which had 297.8 new cases per 100,000 residents during that time.
And Texas looks like a paragon of health compared to Florida, where there were 653.8 new coronavirus cases per 100,000 residents in those same seven days. All of those figures come from the CDC.
We shouldn’t get bent out of shape about every single infection, but what about the more serious cases of COVID-19 that cause patients to seek hospital care?
Over the course of the week, California reported an average of 772 new hospital admissions per day. In the same week, Texas averaged 1,403 new COVID-19 hospitalizations per day and Florida averaged 2,071.
For a little more evidence that mask mandates are helping, consider this: During the first week of August, L.A. County reported 20,979 new coronavirus cases. That represented a 6.5% increase from the previous week — higher to be sure, but in terms of growth it was better than the 22% increase the week before.
The 6.5% figure also looks good when you consider that the number of new coronavirus cases throughout the state was 20% higher during the first week of August than during the last week of July — and the number for the last week of July was 57% higher than the week before.
Of course, it’s far too soon to conclude how much — if any — of the credit should go to mask mandates. Researchers will have to work to disentangle their effects from those of vaccines, past infections, testing programs, school reopenings and other factors. That will take time.
It’s also possible that the divergence in mask policies and coronavirus outcomes is a pure coincidence. As scientists often say, correlation does not imply causation.
Still, I’d rather be in California than Texas, where hospitals are being asked to postpone elective medical procedures. Dr. Natasha Kathuria, an emergency room physician in Austin who has sent patients home because she didn’t have the bandwidth to treat them, said she hears from colleagues in her native Florida that conditions there are even even worse. She’s worried that Texas will soon be following in Florida’s footsteps.
“This is disaster medicine,” Kathuria said. “We’ve never felt this disheartened during the pandemic.”
By the numbers
California cases, deaths and vaccinations as of 5:07 p.m. Friday:
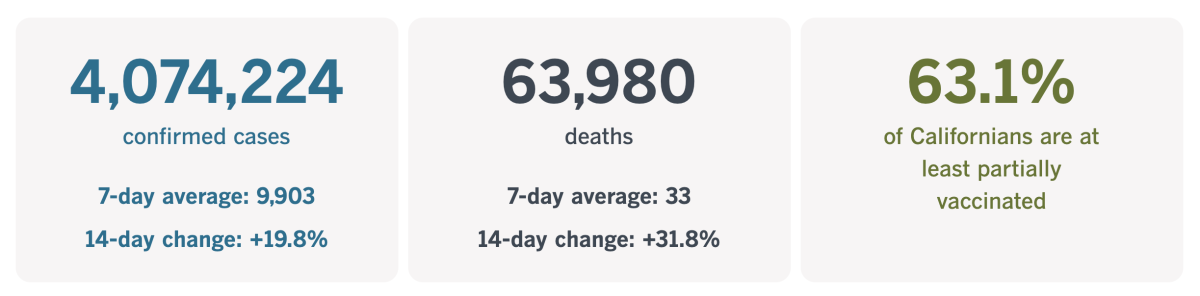
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
What Native Americans can teach us about COVID-19 vaccines
Vaccine hesitancy is a problem throughout the country — after all, more than 40% of Americans who are old enough for the COVID-19 shots still aren’t fully vaccinated — but if you had to pick a group of people for whom the shots would be a tough sell, Native Americans might be high on your list.
They’ve got legitimate reason to be wary of anything the government says is good for them. On top of that, they’re often far from hospitals and other healthcare facilities, and nearly 1 in 4 live in poverty — a higher proportion than any other racial or ethnic group in the U.S.
Reasons like this had health experts bracing themselves for some hard work. Even some tribal leaders had low expectations.
“There is going to be pushback to this vaccine,” Jonathan Nez, president of the Navajo Nation, predicted in December.
But once again, the pandemic threw them a curve, albeit a welcome one: It turns out Native Americans have the highest COVID-19 vaccination rate in the country.
More than 100 million Americans provided their race or ethnicity when they got their shots. That data suggests that Native Americans are 24% more likely than whites, 31% more likely than Latinos, 64% more likely than Black Americans and 11% more likely than Asian Americans to be fully vaccinated.
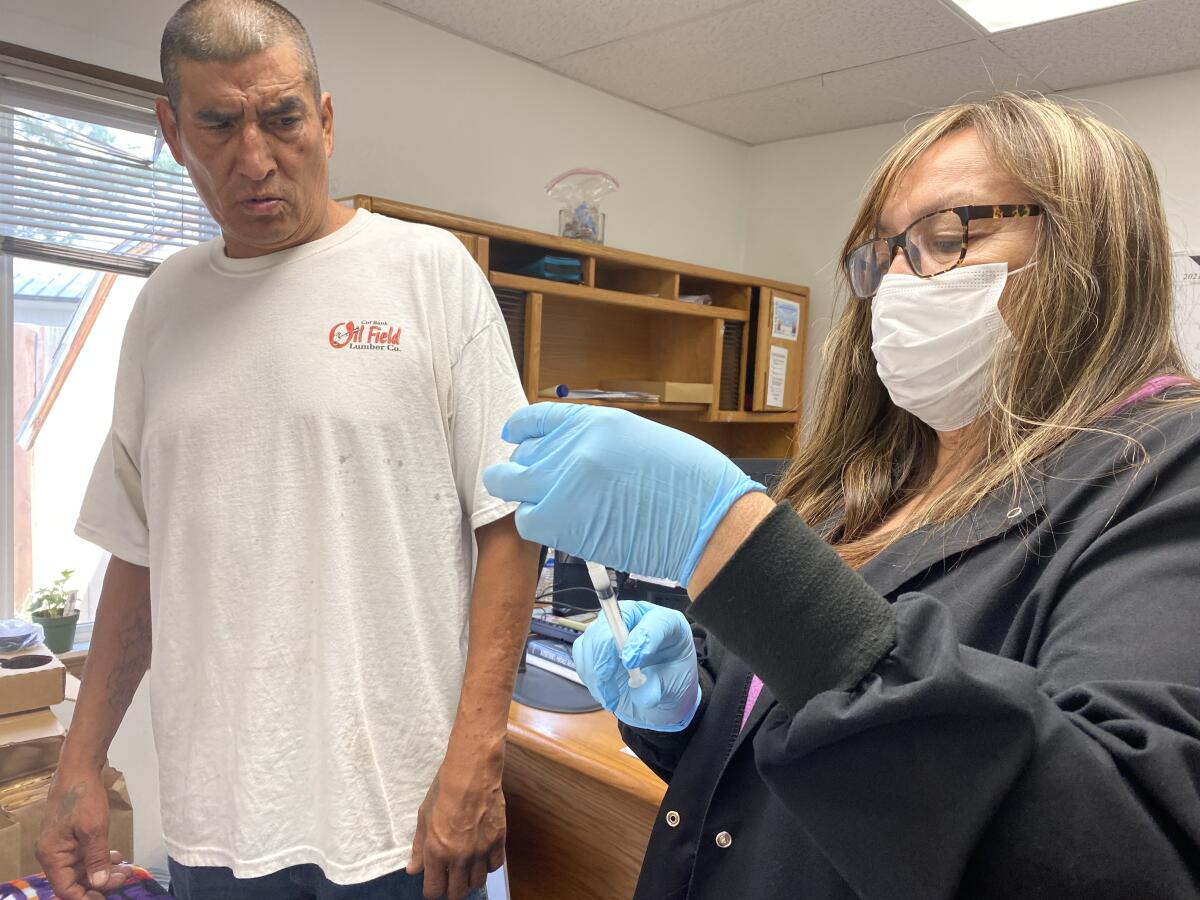
How did they do it? My colleague Richard Read visited the Fort Belknap Indian Reservation in Montana to find out.
One of the keys to success was the recognition by tribal leaders that vaccines offered the clearest, safest path out of the pandemic. And they framed vaccination as a way to protect tribal elders, who were particularly vulnerable to serious cases of COVID-19 due to their high rates of diabetes, heart disease and obesity. (In doing so, they seem to have headed off the conspiracy theories and other forms of vaccine misinformation that took off elsewhere.)
The messages were spread via social media and on the radio. To motivate people, tribes reminded people that COVID-19 had killed Native Americans at a rate 2.4 times higher than for white Americans.
“You’ve got to have armor, and the armor is the vaccine,” Nez said.
That message was received. In a poll of Native Americans, 75% said they would get vaccinated, and that their primary motivation was “a strong sense of responsibility to protect the Native community and preserve cultural ways.”
Tribal health workers pushed hard as soon as the vaccine became available, and they were able to set their own priorities for administering the shots. At Fort Belknap, health workers got them first, followed by essential workers and elders. They also prioritized teachers and other workers at schools attended by Native children — a fortuitous decision, since staffers were partially vaccinated when one of the schools had a sizable outbreak in January.
Tribal leaders got the shots early, to bolster confidence in the vaccine and demonstrate that it was safe.
Now, among the 3,500 people served by the Indian Health Service at Fort Belknap who are old enough to get a vaccine, 67% are fully immunized. That compares with a mere 40% in neighboring Phillips County and 59% for the country as a whole.
The country’s largest tribe, the Navajo Nation, says that more than 70% of its vaccine-eligible members are fully vaccinated.
“This has been just a tremendous effort across all of Indian Country to take care of our people,” said Dr. Loretta Christensen, a member of the Navajo Nation and the chief medical officer of the federal Indian Health Service.
Hopefully, public health leaders elsewhere will learn from that success, said Latoya Hill, a senior analyst at the Kaiser Family Foundation.
“I think it can serve as a model for broader vaccination efforts across the country,” she said.
California’s vaccination progress
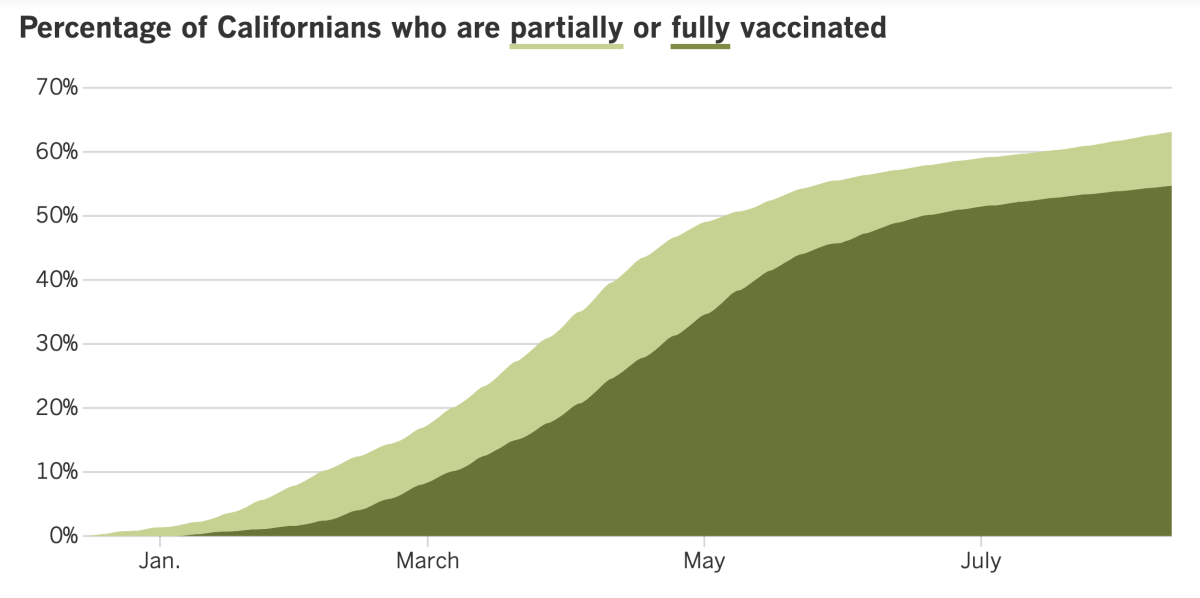
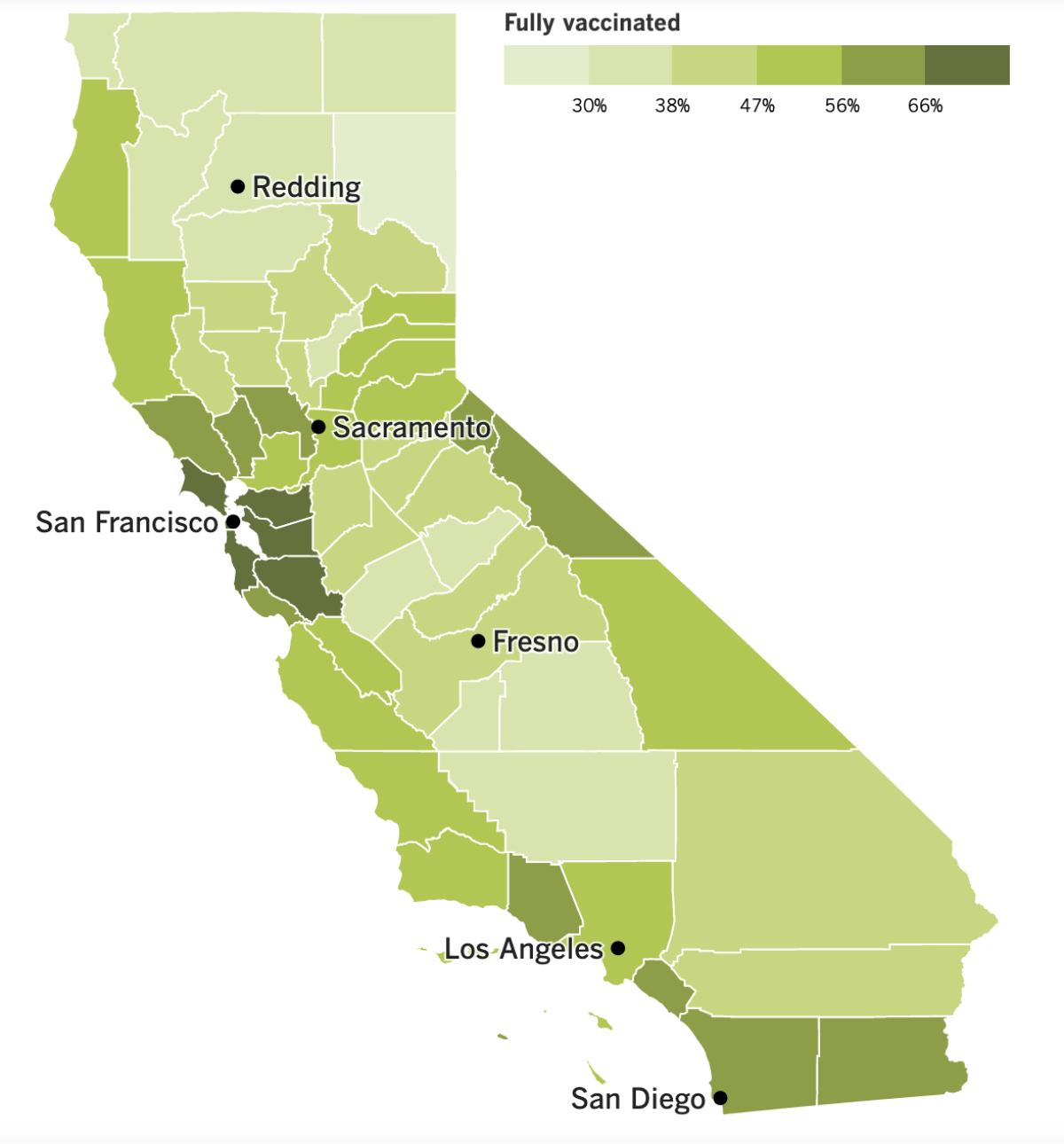
See the latest on California’s vaccination progress with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
In other news ...
Students returned to school this week, and in California, that meant wearing masks on campus. By and large, kids have dealt with the face coverings just fine. But the same can’t be said for all their parents.
Dozens of parents gathered in downtown Chino this week, waving signs demanding to “Unmask our kids” and “Let them breathe.” In Amador County, east of Sacramento, one parent allegedly assaulted a teacher over the face-covering rule.
K-12 students can be exempted from the statewide mask mandate if they have legitimate medical, mental health or accessibility reasons. But some parents are concerned that masks will hinder their children’s social growth, or cause them to overheat. Some object to the mandate on principle.
“It’s about respect, and it’s about a parent’s right to choose what’s right for their kids,” one woman told KTLA.
Torie Gibson, superintendent of the Amador County Unified School District, said the parents she serves were polarized over masks.
“There’s just no middle ground: Either people are super supportive of it and have no issues with it, or they’re completely, adamantly against it,” Gibson told my colleague Hayley Smith.
The backlash isn’t limited to California. A mask mandate for Las Vegas-area schools prompted a lawsuit from attorneys seeking class-action status. They claim the mandate violates the constitutional rights of thousands of parents and children.
The American Academy of Pediatrics strongly endorses universal masking in schools, especially since students under 12 are not yet eligible to be vaccinated against COVID-19. The AAP noted that the number of new coronavirus infections in children nationwide increased last week to 94,000, more than double the number from two weeks earlier.
Teachers and other employees of the L.A. Unified School District will be subject to another mandate. Interim Supt. Megan Reilly said Friday that workers in the nation’s second-largest school system must be vaccinated by Oct. 15.
The vaccine mandate is intended to reassure parents that their children will be safe on campus. It was endorsed by United Teachers Los Angeles, the union representing more than 30,000 teachers, nurses, counselors and librarians. A similar vaccine mandate was approved earlier in the week by the board of the Santa Monica-Malibu Unified School District.
The L.A. City Council moved closer to implementing a vaccine mandate of its own. Members voted Wednesday to have city attorneys draft a law that would require people to have at least one dose of a COVID-19 vaccine before entering an indoor restaurant, bar, gym, shop, movie theater or other venue.
Many details of the proposed law have yet to be worked out, including exactly where it would apply and how it would be enforced. Once decided, the rules would go back to the City Council for a final vote. L.A. previously said it would require city employees to either provide proof of vaccination or submit to weekly testing.
San Francisco is moving ahead with a vaccine mandate of its own. Beginning Aug. 20, patrons of gyms, restaurants, bars and other indoor venues will need to present proof that they’re fully vaccinated before they can enter. Employees will also be subject to the mandate, effective Oct. 13.
A negative coronavirus test result will not be an acceptable alternative under the policy announced Thursday by Mayor London Breed.
“We know that for our city to bounce back from the pandemic and thrive, we need to use the best method we have to fight COVID-19, and that’s vaccines,” she said, adding that the mandate has the support of the city’s business community.
On the national front, the CDC urged pregnant women to get vaccinated against COVID-19. The new advice was prompted in part by safety data revealing that the miscarriage rate for women who received at least one dose of either the Pfizer-BioNTech or Moderna vaccine in the first 20 weeks of pregnancy was around 13%, which is within the normal range.
Only about 23% of pregnant women have been vaccinated, according to the CDC, even though such women run a higher risk of severe illness and pregnancy complications if they come down with COVID-19. The agency had previously encouraged pregnant women to consider vaccinations but stopped short of a full recommendation.
The new vaccination advice also applies to women who intend to become pregnant and to nursing mothers. It echoes the guidance from top obstetrician groups.
Meanwhile, the Food and Drug Administration said Thursday that transplant recipients and other people with severely weakened immune systems can get a third dose of the Pfizer-BioNTech or Moderna vaccine. The decision affects several million Americans, and is in line with policies in France, Israel and several other countries.
People whose immune systems are suppressed by medications and diseases have a harder time responding to vaccines, and small studies have suggested that an extra dose can help. The FDA said qualified people can receive a third dose at least 28 days after their second shot.
There was no mention of immune-compromised patients who received the single-dose Johnson & Johnson vaccine.
Some scientists are pushing back on claims made by Pfizer about the value of booster doses of its vaccine. The company said it would seek FDA authorization for booster shots, but it has not yet delivered conclusive proof to confirm that they will help, especially against the Delta variant.
The pharmaceutical industry’s rush to recommend boosters is “a little frustrating,” said Dr. Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia. Even if boosters are safe, he said, the U.S. effort should still focus on “vaccinating people who are unvaccinated.”
Dr. Sadiya Khan, an epidemiologist and cardiologist at Northwestern University Feinberg School of Medicine, agreed. She said the drive to deliver booster shots is premature while the virus is still circulating among millions of unvaccinated people — the ones responsible for “the overwhelming majority” of infections, hospitalizations and deaths.
“Giving up on that greater strategy of vaccinating the population is going to lead to continued surges,” Khan said. “The potential for harm is quite large.”
And here’s something that’s unlikely to ever happen here: Australia’s capital city began a weeklong lockdown Thursday after a man — just one — was found to be infected with the coronavirus.
Officials don’t know how the Canberra man became infected, but the virus was detected in the city’s wastewater. It was the first locally acquired case since July 10 of last year.
As a result, Canberra retail stores are closed, residents can leave their homes only for essential reasons, and restaurants can only fill orders for takeout. Melbourne, Sydney and several other Australian cities are also in lockdown due to the Delta variant.
Your questions answered
Today’s question comes from readers who want to know: How will schools keep students safe as they reopen?
Both the CDC and the L.A. County Department of Public Health recommend a “layered” approach to safety. That means relying on a variety of measures instead of counting on a single silver bullet. These layers include:
- Face masks. California has implemented a universal mask mandate for all K-12 students while they’re indoors. Exceptions will be rare and hard to get. Some districts, including L.A. Unified, also require masks outdoors.
- Vaccines. Vaccination is strongly encouraged for all teachers and school staff. Those who are not vaccinated must submit to weekly coronavirus testing. The shots are also advised for students who are old enough to get them.
- Physical distancing. There is no minimum requirement for distancing, but schools are being asked to keep students as far apart as possible, especially when they are eating or not wearing masks for other reasons.
- Ventilation. Schools should be optimizing air flow in indoor spaces, ideally by installing high-grade MERV-13 filters on HVAC systems. If those filters can’t be used, portable air purifiers and open windows can help.
- Cleaning. School facilities are supposed to be cleaned frequently, and the people in them will be encouraged to clean their hands often with soap and water or sanitizer.
- School supplies. Sharing will be limited as much as possible.

Got more questions about going back to school in the midst of the Delta surge? Check out our comprehensive guide here.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

This photo of a COVID-19 patient walking across her hospital room with the help of a physical therapist feels like a throwback to an earlier time in the pandemic when hospitals were overwhelmed with coronavirus victims. Unfortunately, it was taken this week at a medical center in Louisiana, where patients are once again so plentiful that a doctor who normally treats people with epilepsy has been pressed into service changing sheets, emptying trash cans and wheeling patients to the radiology department.
Dr. Robin Davis comes in on her days off so that overworked nurses can get a little relief. And boy do they need it: Dozens of rooms in the intensive care unit alone are occupied by pallid COVID-19 patients hooked up to ventilators and beeping machines. In some parts of the state, people seeking treatment for heart attacks and strokes are being turned away from hospitals.
A year ago, Davis felt helpless as she watched friends and neighbors die. This time she’s frustrated because so many of these illnesses could have been averted with vaccines. Only slightly more than 37% of Louisiana residents are fully inoculated.
The earlier waves of victims “were people that didn’t have a chance,” Davis said. “There was nothing we could do to stop this for them. You’ve got a chance now. You have something that gives you the opportunity to have a fate that isn’t like theirs. Please don’t squander it.”
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the state’s COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




