Coronavirus Today: Where did the pandemic start?
Good evening. I’m Karen Kaplan, and it’s Friday, Nov. 19. Here’s the latest on what’s happening with the coronavirus in California and beyond.
More than 250 million people around the world have been infected with the coronavirus. Who was the first, and how did it happen?
We may have gotten closer to the answer this week, thanks to the detective work of evolutionary biologist Michael Worobey. He combed through medical journals, documents from the World Health Organization, news reports and myriad online accounts to reconstruct the early weeks of the outbreak.
Call it “CSI: Wuhan.”
One of the most interesting things he learned was that a Dec. 8, 2019, illness that had been considered the earliest known case of COVID-19 probably wasn’t. The 41-year-old accountant who reported a fever on that date got it as a result of dental surgery to remove baby teeth that never fell out. (A Chinese investigative reporter figured this out.)
The accountant came down with another fever eight days later, which may indeed have been a symptom of COVID-19. Looking back, he said, he suspects be became infected while getting the dental treatment.
With the Dec. 8 fever out of the running, the next candidate for earliest known case of COVID-19 came along on Dec. 11. A difference of three days isn’t necessarily a big deal, but what’s important is that the Dec. 11 patient was a seafood vendor at the Huanan Market, a place where live animals were sold.
That provides a direct link between the earliest known patient and the market that has been under suspicion as the origin of the pandemic. The accountant provided no such link — a fact that caused some people to put less stock in the idea that the coronavirus first jumped from animals to humans at the market.

The most prominent alternative explanation is that the virus was either brought to or created at the Wuhan Institute of Virology, then released into the community either deliberately or by accident.
Worobey was one of 18 researchers who signed an open letter in May that called for a closer look into the possibility that the coronavirus emerged from the lab. Now he’s done it himself, and the evidence he’s collected points away from that scenario.
Among other things, he identified 19 early cases of probable COVID-19 and determined that 10 of them — or 53% — had a link to the Huanan Market. All of those cases were documented before Chinese officials first pointed their fingers at the market, which means the 53% figure could not have been biased by a government trying to deflect attention from the virology lab.
“There was a genuine preponderance of early COVID-19 cases associated with Huanan Market,” Worobey wrote Thursday in the journal Science.
As for the nine cases that weren’t linked to the market, most involved patients who lived close to the market. That’s consistent with the idea that the virus had been circulating in the area for weeks — often among people with few or no symptoms — by the time doctors noticed anything unusual.
Dr. Marc Suchard, a researcher at UCLA who uses genetic sequences to study the spread of disease, said the facts Worobey gathered made clear the Huanan Market was “an early epicenter” of the coronavirus outbreak.
Unfortunately, the case may never get much stronger than that. As we now know, the SARS-CoV-2 virus can be spread by people without making them sick. That means there aren’t medical records for a lot of the folks who helped get the pandemic off the ground.
The Huanan Market was closed and disinfected on Jan. 1, 2020, so any evidence that might link specific animals to the virus is long gone. (Chinese researchers collected samples from 188 animals at the market, but all of them tested negative.)
It’s still possible that, with further work, researchers will be able to learn more about the coronavirus’ origins. Even if they can’t pinpoint the pandemic’s “patient zero,” they should keep digging, Worobey argued.
“Preventing future pandemics depends on this effort,” he wrote.
By the numbers
California cases and deaths as of 4:20 p.m. Friday:
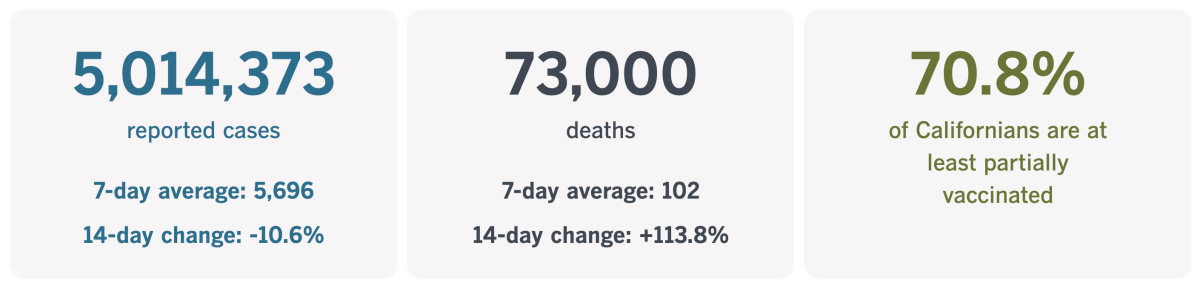
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Gathering for the holidays without sacrificing safety
By this time next week, Thanksgiving will be over, Hanukkah will be just two nights away, and Christmas, Kwanzaa and New Year’s will be here before you know it. After the limits of last year’s holiday season, you may be ready to make up for lost time with extra-large gatherings of family and friends.
The more people in your group, the greater the odds that at least one member is at particularly high risk of developing a serious case of COVID-19. You can protect your vulnerable loved ones by getting vaccinated (and, if warranted, getting a booster shot). You can also reduce their odds of exposure by taking advantage of rapid at-home testing kits.
These kits weren’t around last year, so you might not be familiar with the best way to use them. Luckily for you, my colleague Jon Healey has you covered.
For the most part, rapid tests don’t detect active coronavirus infections — especially new ones — as reliably as tests sent off to a lab. But remember: Your primary goal is to flag folks who might spread the virus to others. If your viral load is high enough for you to be contagious, it’s probably high enough for a rapid test to be able to tell that you’re infected and should stay at home until you recover.
About a dozen different rapid tests have received emergency use authorization from the Food and Drug Administration, although not all of them are readily available for purchase right now. The ones you’re most likely to find are so-called antigen tests. As the name implies, they look for antigens, which are proteins capable of spurring the immune system into action. (Once an infection clears, the antigens are gone.)
The tests typically require you to swab the inside of both nostrils to gather a suitable sample. Then the swab is joined with a test strip and a liquid reagent. Within about 15 minutes, your result becomes visible on the test strip.

If your guests are slated to come over for a holiday meal, it would make sense for them to take a rapid test at home a few hours before they set off. That way, they’ll get a close-to-real-time assessment of their contagiousness and simply stay home if necessary.
If your guests are coming for a longer visit, repeat testing would be a good idea. The first test should be done just before arrival. The second should follow a day or two later, in case the visitor was actually infected the first time around but hadn’t yet built up enough virus — and antigens — to trigger a positive result. (This is why the kits are sold as two-packs.)
Also, experts agree that people who are unvaccinated should test themselves more than once to make sure their results are accurate.
For the most part, prices for rapid antigen tests range from roughly $14 to $35 for a two-pack. Depending on the size of your gathering and the vaccination status of of your guests, the cost for pre-party testing could easily exceed $100.
That might not be worth it if everyone on your guest list is vaccinated and in good health, experts say — especially if you and your guests are in places where coronavirus transmission rates are low.
For more detail about specific tests — including where to buy them and how much they cost — be sure to check out Healey’s story.
California’s vaccination progress
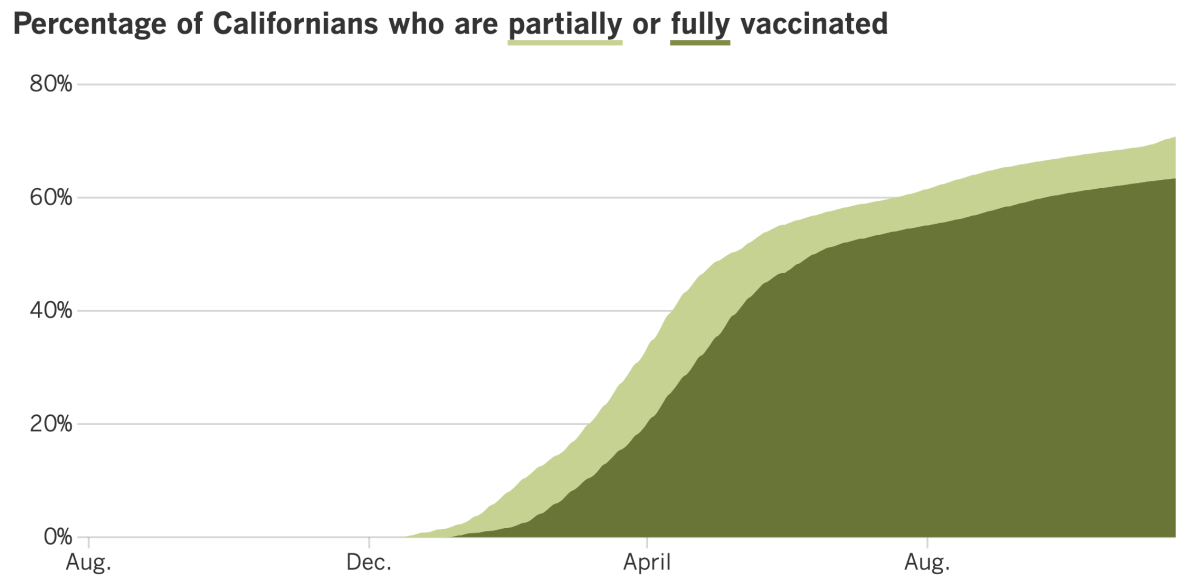
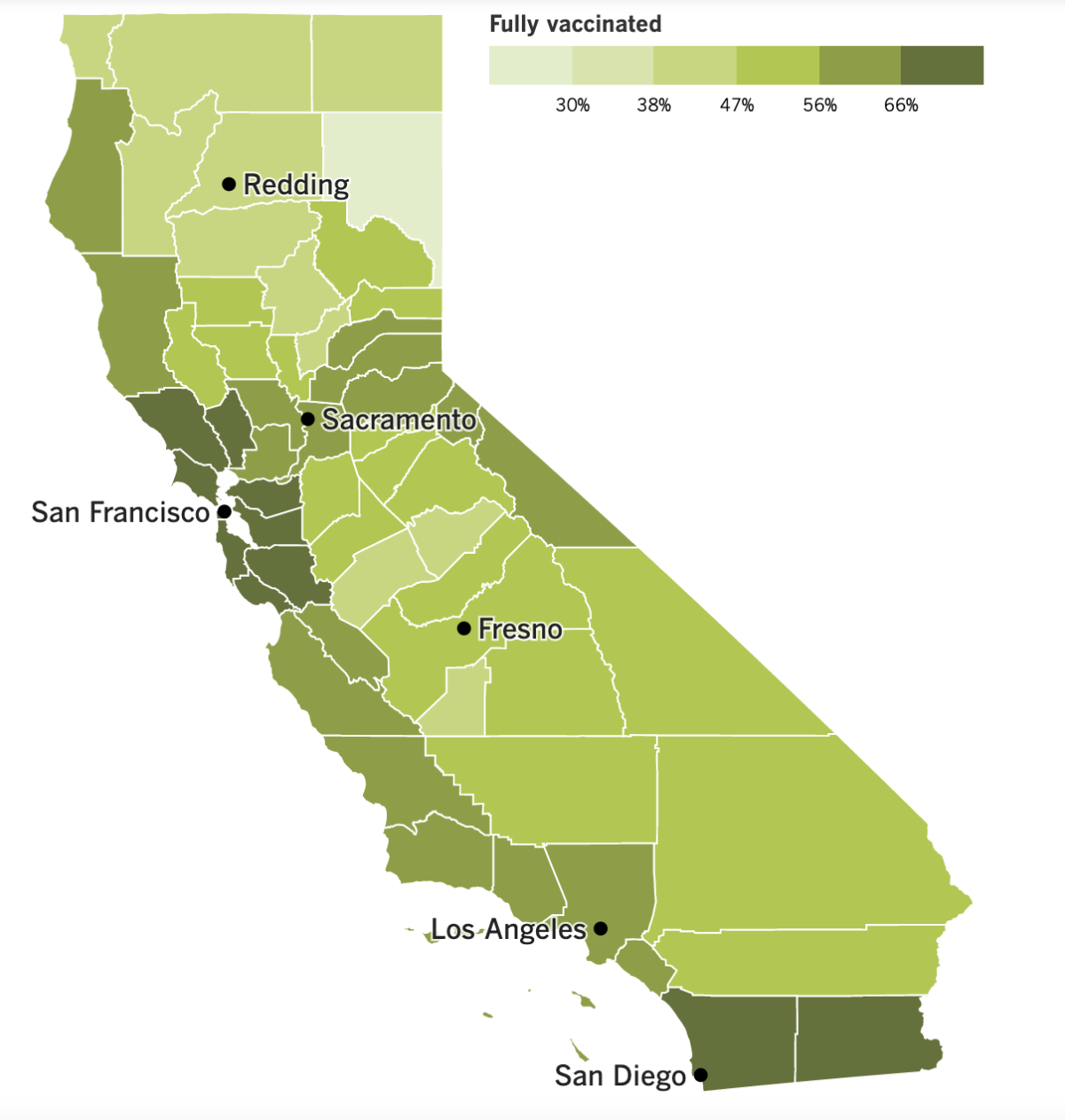
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
The U.S. is catching up to California and nine other states that have made COVID-19 booster shots available to all adults as long as sufficient time has passed for them to qualify.
Both the Food and Drug Administration and the Centers for Disease Control and Prevention gave clearance Friday for broader booster use. That means it’s no longer necessary to consult a complicated checklist to figure out if your job circumstances, living arrangements or medical history make you eligible for the tuneup dose.
Now, all you need to ask yourself is whether you are at least 18 years old and whether it’s been two months since your single shot of the Johnson & Johnson vaccine or six months since your second dose of the Pfizer-BioNTech or Moderna vaccine. (People who are immunocompromised don’t have to wait that long.) So long as you meet those requirements, you are free to get a booster — and to pick which type of booster to get. (Here are some of the things you should consider.)
Health officials hope the new approach to booster shots will encourage more Americans to get them, especially before colder weather and holiday gatherings have a chance to spark another COVID-19 surge. According to the CDC, 70.7% of American adults are fully vaccinated, but only 17.8% have received a booster shot. Not all fully vaccinated adults are booster-eligible, but officials say tens of millions of Americans who could get another dose have not yet done so.
It’s gotten easier for Californians to schedule their booster shots now that the state’s MyTurn appointment scheduling tool has stopped asking questions about eligibility. As of Thursday, people who received the Pfizer and Moderna vaccines no longer have to say whether they’re in a high-risk group before making an appointment.
The questions posed on MyTurn.ca.gov were in line with the CDC’s previous booster criteria, even though state officials had declared that no one who wanted another dose would be denied one as long as they met the simple time requirements. Some people found themselves in the uncomfortable position of having to lie in order to schedule a shot.
Here’s a number that might encourage some Californians to get a booster shot sooner rather than later: 5 million. That was the state’s coronavirus case count as of Thursday morning. (It’s now up to 5,014,373.)
At the time that milestone was reached, about 4.75 million of those infections had been confirmed with PCR tests. The rest of them were “probable” cases that were identified with an antigen test.
No other state has recorded as many infections, but keep in mind that no other state has nearly as many residents. California’s cumulative infection rate is about 12,775 cases per 100,000 people, the 10th-lowest among all states.
Back in Washington, the U.S. government has made a deal to buy 10 million courses of Pfizer’s experimental COVID-19 pill — if it passes muster with federal regulators.
Pfizer says its pill, which will be called Paxlovid, reduced the risk of hospitalizations and deaths by 89% for unvaccinated, high-risk adults who began treatment shortly after their first symptoms emerged. The pill’s effectiveness in vaccinated and lower-risk adults remains to be seen.
Under terms of the deal, the 10 million courses will cost $5.29 billion, or $529 per course. The government has already agreed to buy about 3.1 million courses of a similar pill from Merck at a cost of about $700 per course.
Patients won’t have to worry about the cost, however. President Biden assured the public that both treatments “will be easily accessible and free.”
Speaking of federal investments, the Biden administration wants COVID-19 vaccine makers to ramp up their production and is making billions of dollars available to help them to do so.
The goal is to produce an additional 1 billion doses per year, then share them with the rest of the world. Not only would that reduce illnesses and deaths in countries that are still waiting for — and perhaps can’t afford — the shots, but it could also slow the evolution of new variants by depriving the virus of opportunities to mutate.
We have an update from Austria, which attempted to address its latest surge by implementing a nationwide lockdown for unvaccinated residents. Less than a week in, Chancellor Alexander Schallenberg announced the lockdown order would be expanded to all Austrians since cases there have continued to skyrocket.
The broader restrictions will go into effect Monday and last for at least 10 days. Most stores will have to close, cultural events will be canceled, and parents are strongly encouraged to keep their children at home.
That’s not all: COVID-19 vaccinations will become mandatory in Austria on Feb. 1, according to a report from public broadcaster ORF.
Here’s something to bring us all together: A new study that examined phone calls to help lines around the world has found that we have a lot in common when it comes to assessing the pandemic’s toll on our mental health.
Fear of becoming infected, loneliness and concerns about physical health turned up again and again in the analysis of 8 million calls made in 19 countries, including the United States, China, Lebanon and Finland. On the plus side, calls prompted by concerns about suicide, relationship issues and economic problems all became less prevalent.
“We were struck by how similar the broad evolution of helpline call patterns looked across nations,” said study leader Marius Bruelhart, an economics professor at the University of Lausanne in Switzerland. The findings were published Wednesday in the journal Nature.
Your questions answered
Today’s question comes from readers who want to know: What safety precautions should I take if I’m traveling for Thanksgiving?
Thanksgiving travel is expected to be back up to pre-pandemic levels this year. If you’re planning to hit the road, there are steps you can take to reduce your risk of bringing the coronavirus along as an uninvited guest — or home with you when you return.
Here’s some advice from the CDC to help you get around the country safely this holiday season:
- Don’t travel until you’re fully vaccinated.
- If you must travel anyway, the CDC advises that you get tested for an infection one to three days before your departure, then tested again three to five days after you get back. You should also prepare to quarantine at home for seven days if your coronavirus test comes back negative, or for 10 days if you skip the test.
- If you test positive for a coronavirus infection, stay home.
- If you’re not fully vaccinated, you should also stay put if you’ve recently been exposed to someone with COVID-19, unless you’ve recovered from an infection in the past 90 days.
- Wear a mask that covers your nose and mouth while you’re on a plane, train, bus or other form public transportation. You’ll also need that mask while you’re in an airport or other transportation hub. (Masks are not required in outdoor areas, such as the deck of a ferry or the uncovered top of a bus.)
- Check for COVID-19 rules and restrictions at your destination. You don’t want to get there and then realize you needed to bring your CDC COVID-19 Vaccination Record Card but left it at home.
- Wear a mask indoors if you’re not fully vaccinated, if you’re going to a place where coronavirus transmission levels are “substantial” or “high” (you can check that here), or if you have a weak immune system.
- Don’t forget to wash your hands or use hand sanitizer frequently.
Have fun!
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

The photo above was taken Tuesday at Griffith Observatory in Los Angeles in advance of a memorial to honor people who have died of COVID-19. The lawn in front of the observatory is studded with 27,000 white flags — roughly one to honor each victim from L.A. County.
The three-day memorial combines virtual and in-person events and ends Saturday. For information about how to participate, visit the city’s website for Strength and Love, the City of Angels’ COVID-19 Memorial.
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if you’re eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get tested? Here’s where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




