Coronavirus Today: Giving up on vaccine mandates
Good evening. I’m Karen Kaplan, and it’s Tuesday, June 7. Here’s the latest on what’s happening with the coronavirus in California and beyond.
It sounded like just the kind of thing you’d expect from lawmakers in a blue state where Democrats hold veto-proof supermajorities in both houses of the legislature: a bundle of bills designed to get more Californians vaccinated against COVID-19.
The bills aimed to make it easier to check vaccination records, counter misinformation about the shots, and allow adolescents to get vaccinated without their parents’ consent, among other things.
The centerpiece of the package was a pair of bills that would have established vaccine mandates for most Californians. One was written to make workers — both employees and independent contractors — get the shots if they worked indoors unless a valid medical condition, disability or religious belief prevented it. The goal of the other was to add the COVID-19 vaccine to the list of childhood immunizations K-12 students needed to attend school in person, unless they had a legitimate medical exemption.
“None of us want to go back to closing down schools or closing down businesses,” said Assemblywoman Buffy Wicks (D-Oakland), a sponsor of the legislation. “We know if we’re vaccinated, we can combat this.”
Fast-forward several months. Today, only the teen vaccine consent bill is still up for consideration (it passed in the Senate and is making progress in the Assembly). The rest of the measures were withdrawn before they even came up for votes.
Why did this ambitious effort to promote COVID-19 vaccines fizzle out so fast?
Anti-vaccine activists were vocal in their opposition, but that was hardly a deciding factor, our friends at Kaiser Health News reported.
“I don’t think the anti-vaxxers carry much weight in Sacramento with my colleagues,” Wicks said. “They’re a pretty insignificant part of the equation.”

Labor unions representing law enforcement officers and firefighters held more sway. They argued that a blanket mandate for workers would deprive local bargaining units of the chance to negotiate their own deals regarding vaccination. Many of their members were vehemently opposed to the idea that they would be forced to get vaccinated. (In Los Angeles, where a citywide vaccine mandate was implemented, some L.A. Police Department officers turned in their badges to avoid the shots.)
Small-business groups welcomed the idea of a single statewide vaccine mandate because it would be more straightforward than managing myriad local requirements. But other businesses saw things differently, as did some of the legislature’s more moderate Democrats.
By the end of March, the bill was shelved before it even got a hearing.
The bill that would have strengthened the vaccine mandate for schools was short-lived as well.
Gov. Gavin Newsom had already added COVID-19 shots to the list of vaccines California students needed to get to attend school. But since that policy was implemented through an executive order instead of a law, it came with a loophole: Parents could opt out by claiming a “personal beliefs” exemption. Closing that loophole was the purpose of the bill.
The legislation was introduced during the Omicron surge, when the state was recording more than 100,000 new coronavirus infections each day. After the wave subsided, the case for a strong mandate was more difficult to make.
Indeed, improving COVID-19 conditions sapped the political will to implement vaccine mandates of any kind.
“It’s hard to make that argument that right now we need to be mandating when you have a good number of people who feel like we are past the pandemic,” said Assemblymember Akilah Weber (D-San Diego).
That statement is notable for two reasons: Weber was one of the initial supporters of the package of COVID-19 bills, and she is a physician.
Catherine Flores-Martin, executive director of the pro-vaccine California Immunization Coalition, suggested that it would take another big surge to revive the scuttled bills — but by then, it would be too late to head off a new wave of illnesses.
“I’m disappointed that people are not taking the long view,” she told Rachel Bluth of Kaiser Health News.
Hemi Tewarson, executive director of the National Academy for State Health Policy, is even more pessimistic. She fears rising cases won’t be enough to prompt action on COVID-19 vaccines now that so many people have adopted the mindset that the pandemic is pretty much over.
There is one kind of vaccine bill that’s popular with state legislatures: measures that prevent COVID-19 vaccine mandates. At least 19 states have passed such laws, according to Tewarson’s group.
By the numbers
California cases and deaths as of 4:20 p.m. Tuesday:
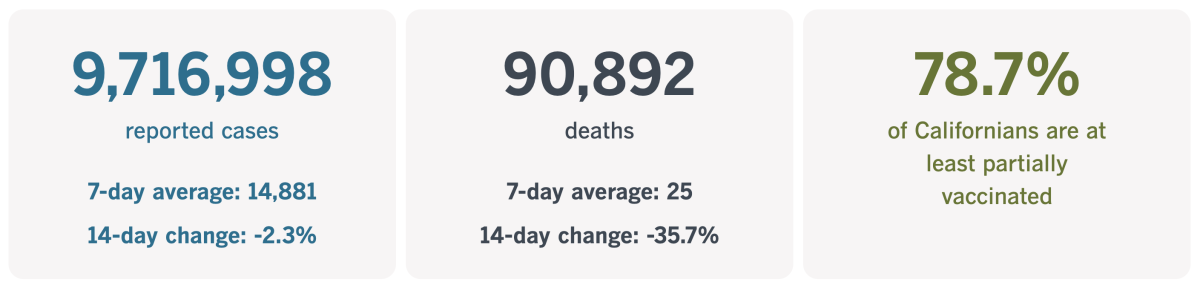
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Lessons from the tobacco wars
The U.S. Surgeon General’s office published its first comprehensive scientific report laying out the health risks of smoking in 1964. After combing through more than 7,000 studies, a committee of experts concluded that smokers had a 70% higher mortality rate than nonsmokers, and that their cigarette use was to blame.
At the time, nearly half of American adults were cigarette smokers — and the tobacco industry was keen to keep it that way.
Tobacco companies fought back by raising doubts about the science that informed the report and countered it with misinformation of their own. They criticized attempts to curtail smoking as threats to individual freedom. And they suggested there would be steep economic consequences if the government attempted to insert itself in the industry’s affairs.
Sound familiar?
It does to a trio of public health and public policy experts who are interested in getting more Americans to embrace COVID-19 vaccines.
Go online and it’s easy to find “vast amounts of misinformation about vaccine safety and effectiveness,” the three write in an essay that will be published in this week’s print edition of the New England Journal of Medicine. “Social media and right-wing media channels now promote conspiracy theories that vaccines deliver microchips to control behavior, render vaccinees sterile, or harm fetuses.”
That’s not all. The attacks on Dr. Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, are reminiscent of the attacks on Dr. C. Everett Koop, the surgeon general whose 1986 report arguably turned the tide in the fight against Big Tobacco. And with both smoking and vaccines, important public health disputes are being resolved by judges without expertise in medicine or epidemiology.
Today, the smoking rate among U.S. adults is 12.5%, the lowest it’s ever been. The story of how cigarette use went from normal — even glamorous — to just barely socially acceptable could provide a roadmap for changing Americans’ attitude towards COVID-19 vaccines.
The essay authors — Robert Bazell, a science and technology policy fellow at Yale; Dr. Howard Koh, a Harvard professor with expertise in public health leadership; and Barry Bloom, an immunologist and health policy expert at Harvard — argue that Koop’s report changed the public’s attitude toward tobacco by showing that people who choose to smoke affect the health of those who choose not to smoke.
“What was initially a concern specific to smokers became everyone’s problem when the public understood that one person’s actions endangered other people’s lives,” the trio write.

Seen through that lens, it became imperative to prohibit smoking in offices, restaurants, airplanes and other public places. And once smoking was seen as something to discourage, it made sense to slap sin taxes on cigarettes, set limits on marketing, and broadcast public service announcements featuring sickly smokers who wish they’d never picked up the habit in the first place.
COVID-19 vaccines are the flip of cigarettes: The goal is to shift skeptics’ perception of them from fringe and scary to commonplace and expected. But Bazell, Koh and Bloom say the methods for pulling off this image makeover can be the same, including:
• A public relations campaign to drive home the point that people who aren’t vaccinated put their families, friends and communities in danger.
• A series of PSAs starring severely ill COVID-19 patients who say they wish they’d gotten the vaccine. (There’d be no need to hire actors.)
• A separate public information campaign featuring doctors and nurses explaining how COVID-19 patients burden the healthcare system for everyone.
• Laws requiring people to show proof of vaccination to enter schools, shopping malls and other public spaces.
• Vaccine mandates (if anyone has the will to implement them; see above).
The trio also raised the idea of allowing people to sue businesses if their unvaccinated workers cause “harm,” though the U.S. Supreme Court may see that as tantamount to a vaccine mandate for private employers, something they’ve already rejected.
“The roadmap drawn by tobacco-control efforts shows that the public mindset can be tilted toward public health and social good,” they write. “With vaccination, this work shouldn’t take decades; it needs to begin immediately.”
California’s vaccination progress
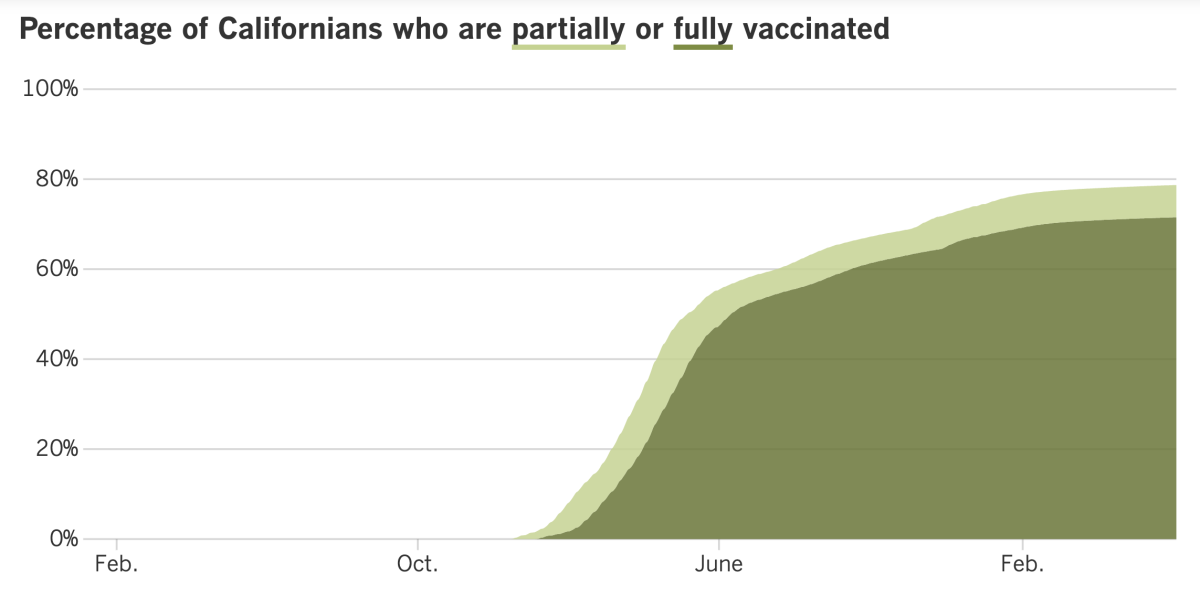
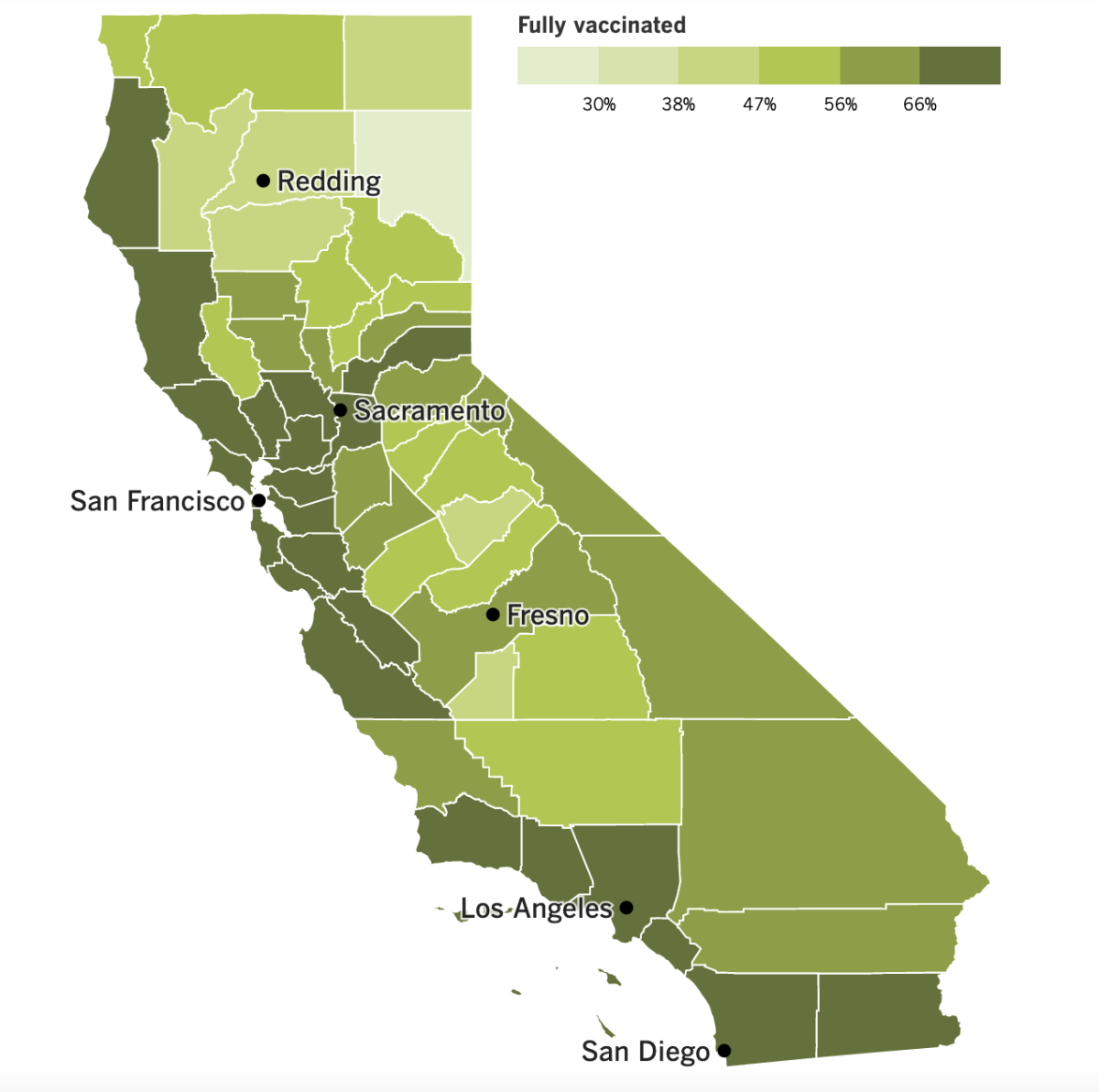
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
Coronavirus infections in California have been rising for weeks, but the mantra has been that as long as they’re not accompanied by dramatic increases in COVID-19 hospitalizations and deaths, there’s little reason to worry.
Now that’s starting to look like wishful thinking.
At a minimum, the long-term upward trajectory in cases is causing disruptions in daily life. Even a mild illness keeps people at home for at least several days, potentially interfering with plans for graduations, weddings and summer vacations. Businesses are back to worrying about staying open with a bare minimum of manpower.
Hospitalizations are on the rise again too. At L.A. County-USC Medical Center, the county’s biggest hospital, only about 10% of the coronavirus-positive patients were admitted because they needed treatment for COVID-19. But all of them require extra hospital resources, in part because they need to be isolated.
“There is no way to get around the reality that surges of COVID-19 are problematic — they result in people being sick enough to be out of work; others sick enough to be in the hospital; others sick enough to have longer term issues,” tweeted Dr. Abraar Karan, an infectious-disease expert at Stanford. “Normalizing surges is bad public health.”
It’s possible that California is already retreating from the brink.
Data released Friday show the 7-day average of new cases across the state dropped 12% compared to the previous week. That works out to 247 cases per week per 100,000 residents — well over the 100 cases per 100,000 that qualifies as a high rate of viral transmission — but it’s the first week-to-week decline in two months.
If last week’s Memorial Day holiday led to a delay in reporting cases, however, it could be a fluke.
“We will continue to monitor this closely to see whether or not we’ve plateaued,” said L.A. County Public Health Director Barbara Ferrer.
In the meantime, mask rules are back on the table in some parts of California.
The Centers for Disease Control and Prevention says counties with high COVID-19 community levels — meaning not just that infections are widespread but that hospitals are in danger of being overburdened — should implement universal indoor masking rules. As of Thursday, 13 California counties are in that tier: Santa Clara, Sonoma, Solano, Marin and Napa in the San Francisco Bay Area; Sacramento, Placer, Yolo, El Dorado in the Sacramento Valley area; and Monterey, Mendocino, San Benito and Del Norte elsewhere in Northern California.
Alameda County, home to Oakland and the second-most populous county in the Bay Area, isn’t on that list. Yet as of Friday, it implemented a mask mandate for most indoor public settings, the first to do so since the original Omicron wave subsided.
“We cannot ignore the data, and we can’t predict when this wave may end,” said Dr. Nicholas Moss, the county’s health officer. “Putting our masks back on gives us the best opportunity to limit the impact of a prolonged wave on our communities.”
Alameda County has a medium COVID-19 community level, with about 354 cases per 100,000 residents per week, according to the CDC. Los Angeles County isn’t far behind, with about 321 cases per 100,000 per week, but the rate of new COVID-19 hospital admissions here is much lower (5.3 versus 9.3 new admissions per 100,000 county residents per week), the CDC says.
Ferrer warned last week that the nation’s most populous county could implement a new universal indoor mask mandate by the end of the month if present trends continue.
“Our weekly case rate and the rate of increase in hospital admissions are of concern,” she said. “If we continue on the current trajectory … we’re likely to move into the CDC high [COVID-19] community level within a few weeks.”
Whether people will be inclined to abide by new mask orders is an open question. If you’ve gone pretty much anywhere recently, you’ve surely noticed that lots of people aren’t swayed by the California Department of Public Health’s stance that face coverings are “strongly recommended” in a variety of indoor settings and on public transit.
In Washington, Biden administration officials say they’re running out of money to buy the latest COVID-19 vaccines, tests and treatments. They’re also low on cash to reimburse doctors who treat uninsured patients, among other things.
The reason is the continued Congressional stalemate over President Biden’s request for more funds to respond to the pandemic. Without additional money, “I think we would see a lot of unnecessary loss of life,” Dr. Ashish Jha, the White House’s point person on COVID-19, has warned.
At least there’s been some progress on COVID-19 vaccines.
Pfizer and BioNTech have asked the Food and Drug Administration to authorize their shots for children between the ages of 6 months and 4 years. The regimen for this age group is a three-dose series, with each dose containing one-tenth the amount of vaccine given to adults.
The FDA’s vaccine advisory committee is scheduled to consider the companies’ application at a meeting next week. Jha said that if all goes well, the vaccine could be offered to infants, toddlers and preschoolers as soon as June 21. The administration already has an initial supply of 10 million doses.
Novavax’s COVID-19 vaccine for adults went before the same FDA advisory committee on Tuesday and received a favorable review. If agency officials authorize it — and the CDC recommends it — people who’ve been holding out for a more traditional type of vaccine will finally have a reason to roll up their sleeves.
“We do have a problem with vaccine uptake that is very serious in the United States,” said Dr. Peter Marks, the FDA’s vaccine chief. “Anything we can do to get people more comfortable to accept these potentially life-saving products is something that we feel we are compelled to do.”
Your questions answered
Today’s question comes from readers who want to know: Should I just get COVID-19 and get it over with?
The longer this pandemic drags on, the more this question comes up — especially among people who’ve been conscientious about evading the coronavirus for nearly 2½ years and fear their luck is bound to run out. The fact that each Omicron subvariant seems to be even more transmissible than the last only adds to the sense of futility.
But the answer to the question is still no.
For one thing, the “get it over with” mindset implies that if you’ve had COVID-19 once, you won’t get it again. Unfortunately, that’s not the case.
A recent study published by the CDC examined coronavirus infections in California between May 30 and Nov. 20 last year, a period when the Delta variant was dominant. Researchers found that 3.6% of vaccinated Californians who caught the virus during that window were experiencing repeat infections, as were 5% of the unvaccinated Californians who were infected during that window.
Numbers like those got worse during the Omicron surge.
The United Kingdom, for instance, posts a daily count of coronavirus reinfections on its website, and it’s clear to see that such cases began to spike in early December, as Omicron began its rapid spread. As of mid-March, the U.K. had documented more than 1.2 million reinfections, most of them in the Omicron era.
A laboratory in Marseille, France, has tracked a cohort of more than 80,000 people since the start of the pandemic. Researchers there observed a 6.8% reinfection rate during the Omicron surge, significantly higher than the 1.5% reinfection rate seen in earlier waves.
Even if none of that were true, it’s still a bad idea to treat COVID-19 like a case of the chickenpox. There’s no guarantee that your coronavirus infection will be mild. As of Tuesday, the U.S. is averaging nearly 3,800 new hospital admissions for COVID-19 each day.
Plus, even a mild case of COVID-19 could result in long COVID, leaving you with symptoms you can’t shake for months — or possibly longer.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

LBGTQ Pride Month is here, and local festivities are back after a COVID-19 hiatus.
The cities of West Hollywood and Venice hosted parades on Sunday. The men above, wearing their law enforcement uniforms, were photographed at the venerable WeHo event.
Singer-songwriter-actress-author Janelle Monáe served as the parade’s grand marshal. Other celebrity participants included rapper Cardi B and reality star JoJo Siwa.
The L.A. Pride Parade is coming up this Sunday at 10:30 a.m. Check out our Pride guide for ways to celebrate all month long.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




