Coronavirus Today: Will an Omicron vaccine prevent another winter surge?
Good evening. I’m Karen Kaplan, and it’s Tuesday, July 12. Here’s the latest on what’s happening with the coronavirus in California and beyond.
Who’s looking forward to a third consecutive winter surge that causes hospitals to fill with COVID-19 patients and sends the death toll spiraling?
Not me. And neither are the good folks at the Food and Drug Administration.
They’re looking to head off another disastrous winter by tweaking the formula for the nation’s COVID-19 booster shots.
The vaccines and boosters currently available in the U.S. were designed with a particular strain of SARS-CoV-2 in mind — one that left China way back in January 2020. Since then, the World Health Organization has recognized five major variants of concern and eight additional variants of interest. According to the Centers for Disease Control and Prevention, all of the coronaviruses now circulating in the United States are some version of the Omicron variant.
In other words, the coronavirus has changed, but our shots haven’t.
So last month, the FDA convened a meeting of its vaccine advisory committee to get advice on how to proceed. Dr. Peter Marks, the FDA’s vaccine chief, told the panel that all options entail some degree of risk.
If the agency decided to update the formula, the new shots would become available without being subjected to the extensive clinical trials used to vet the original vaccines. The agency decided long ago that modifications to COVID-19 vaccines it had already authorized or approved would be evaluated using a streamlined process. In the unlikely event that an update created a safety problem, it would be up to the FDA’s surveillance systems to detect it in a timely manner.
On the other hand, Marks warned, if no changes are made, Americans who are fully vaccinated and boosted could find themselves with significantly less protection than they have had in years past. One study found that three doses of mRNA vaccine offered half as much protection against Omicron as they did against Delta, the variant that preceded it.

If new vaccines are warranted, there’s the non-trivial matter of deciding which strain (or strains) should replace the original. This is a lot trickier than it may sound.
Let’s say you pick BA.5, currently the country’s dominant Omicron subvariant. As of Tuesday, 65% of the coronaviruses spreading in the U.S. were of the BA.5 variety. But a month ago, BA.5 accounted for just 17% of the viruses in circulation, and BA.2.12.1 had a 57% market share. Given how quickly things change, who’s to say whether BA.5 will still be a factor by the time a fall booster campaign gets underway?
Getting a timely and accurate fix on all this “is truly a challenge, and it is science at its hardest,” Marks said.
It sounded more like black magic to Dr. Arnold Monto, the chair of the vaccine advisory committee. “We’re being asked, essentially, to have a crystal ball,” he groused.
A version of this goes on twice a year, when the World Health Organization decides on the composition of the influenza vaccine for the coming flu season. Like the coronavirus, the flu virus changes from year to year, and experts take those changes into account when deciding which strains the flu shot should target.
They don’t always come up with an accurate forecast — and the consequences can be serious. During the 2014-15 season, bad guesses about the influenza A viruses expected to show up in North America diminished the shot’s effectiveness, contributing to 758,000 flu hospitalizations among the elderly and 148 deaths among children, my colleague Melissa Healy reports.
After the advisory committee adjourned its meeting, FDA officials announced their choice: New COVID-19 boosters should prime the immune system to recognize both the original coronavirus strain and the BA.4 and BA.5 subvariants, which share the same spike protein.
The choice has its detractors. Dr. Paul Offit, a committee member from the University of Pennsylvania, said there was insufficient evidence that redesigned boosters would prevent serious illnesses and death more effectively than the current versions, whose safety is well established. Exposing Americans to the risks of a tweaked vaccine “is not OK when those benefits aren’t clear,” he told Healy.
In the long run, the solution is to devise a vaccine that keeps working even as the coronavirus evolves. Ideally, a “universal” vaccine would target some part of the SARS-CoV-2 virus that doesn’t mutate the way the spike protein does, but that’s a lot easier said than done.
Scientists around the world have been pursuing this goal for well over a year. One research group that’s trying to make this happen announced last week that it was making plans to test its candidate vaccine in humans in a Phase I clinical trial.
The team members, from Caltech and Oxford University, created a nanoparticle adorned with pieces of SARS-CoV-2, along with seven related coronaviruses. Mice and monkeys inoculated with the vaccine were protected against a range of viruses, including ones that the shot hadn’t introduced to their immune systems.
“We’ve had three pandemics or epidemics in the past 20 years: first SARS, then MERS, then SARS-CoV-2,” Caltech biochemist Pamela Bjorkman told my colleague Corinne Purtill. More outbreaks sparked by “spillover events” are inevitable, she said, and “we want to protect now against the future spillover.”
By the numbers
California cases and deaths as of 6:10 p.m. on Tuesday:
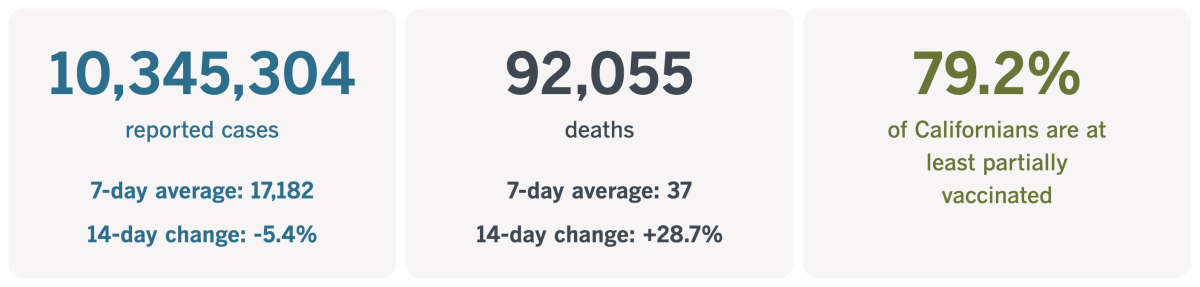
Track California’s coronavirus spread and vaccination efforts — including the latest numbers and how they break down — with our graphics.
Working with COVID-19? Give it a rest
Amid all the talk about Paxlovid, molnupiravir and monoclonal antibodies, there’s one COVID-19 remedy that doesn’t get the respect it deserves.
It’s safe, free and abundant to those who are willing to take advantage of its healing properties.
I’m talking about rest.
Doctors told my colleague Emily Alpert Reyes they were dismayed to see so many COVID-19 patients discount or dismiss their need to rest.
“Sleep equals immunity,” said Dr. Susan Cheng, a cardiologist and researcher at Cedars-Sinai Medical Center. “You want to have your immune system not distracted by anything else” while it’s trying to rid your body of the coronavirus. That includes distractions caused by work.
“You really want your body to recover,” she added. “Give it as much rest as possible, to recover as fully as possible.”
Lest you dismiss Cheng as an outlier, listen to what Dr. Caitlin McAuley, a family medicine specialist at USC’s Keck School of Medicine, had to say.
“Getting adequate sleep lets the immune system rebalance,” she said. “In any acute illness — and COVID especially — we know that rest is important.”
That definitely includes taking a break from work, she added: “At a minimum, you really should unplug for three to five days.”
And if you’re still not convinced, here’s some advice from Dr. Timothy Brewer, an infectious diseases specialist at UCLA.
“Your body is pretty good at telling you what it needs,” he said. “So if you’re feeling tired and you’re sick with COVID, that’s probably your body saying, ‘Get back in bed.’ ”
Sometimes this is easier said than done. Many hourly workers can’t afford to take time off because clocking in is the only way to get paid. Surveys by the Kaiser Family Foundation found that roughly 1 in 10 workers had gone to their jobs after they’d been exposed to the coronavirus or had developed COVID-19 symptoms because they needed the money. People from households with less than $40,000 in annual income were far more likely than their higher-income peers to go to work after an exposure, by a margin of 29% to 6%.
That’s not necessarily unique to COVID-19. Researchers with the Shift Project at the Harvard Kennedy School reported that two-thirds of service workers said they’d worked while ill because they needed to hold on to their jobs. It wasn’t just the income to be gained by powering through a few miserable shifts; it was the fear of being reprimanded or fired if they called in sick.
(This ought to be less of a problem in California thanks to a law that guarantees 80 hours of paid sick leave to workers trying to recover from COVID-19. The benefit is available to people who work in companies with at least 26 employees.)
White-collar employees are guilty of working while sick with COVID-19 too. It’s tempting because the pandemic has made working from home a normal part of life.

Dr. Anthony Fauci assured the nation that he would continue working from his Washington, D.C., home when he contracted a mild case of COVID-19 last month. The following week, while still isolated at home, he donned a suit jacket and tie to join a Senate hearing on the government’s pandemic response via video.
He wasn’t the only government official to prioritize work over rest. Secretary of Transportation Pete Buttigieg pledged to work remotely when he came down with COVID-19. San Francisco Mayor London Breed conducted meetings from home when she tested positive. And when a spokesman for Sen. Chuck Schumer announced Sunday night that his boss had a mild case of COVID-19, he said the majority leader would “continue with his robust schedule and remain in near constant contact with his colleagues.”
Workaholics like these are setting a bad example by “encouraging others to think, ‘If I have the virus, I can just push through it,’” said David Putrino, director of rehabilitation innovation for the Mount Sinai Health System in New York.
If you must work while sick, it’s infinitely better to work from home. But you’d be much better off not working at all. Mental exertion uses energy, and even a partial workload can strain your immune system and hamper your recovery.
It might even make you sicker. Cheng pointed to studies of mice that were infected with run-of-the-mill viruses. Some were forced to swim; others were not. The swimmers fared much worse than their counterparts who were able to rest.
California’s vaccination progress
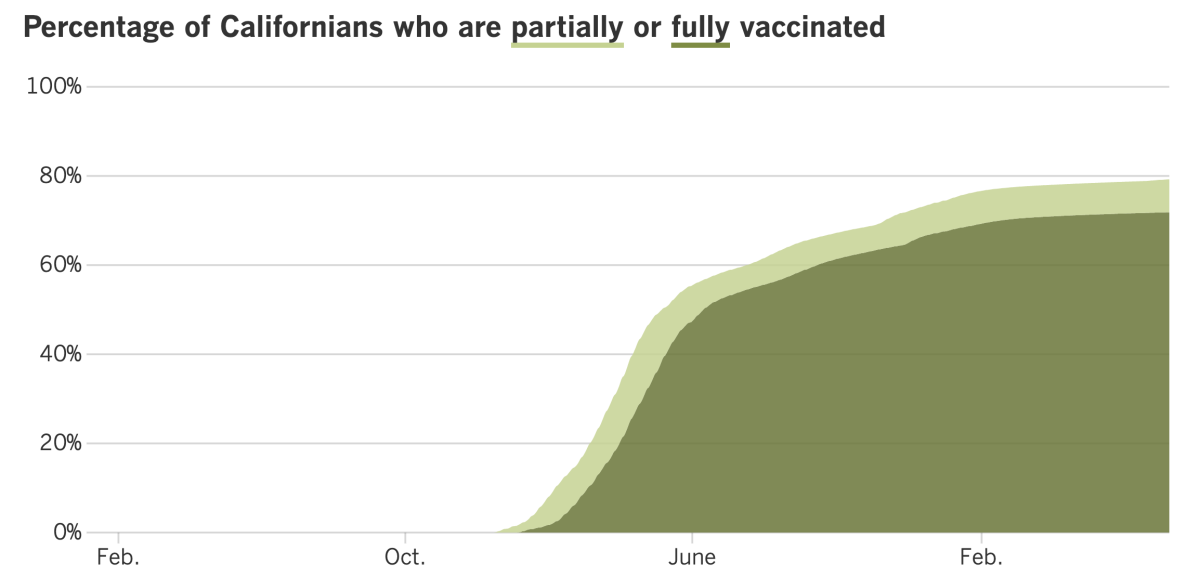
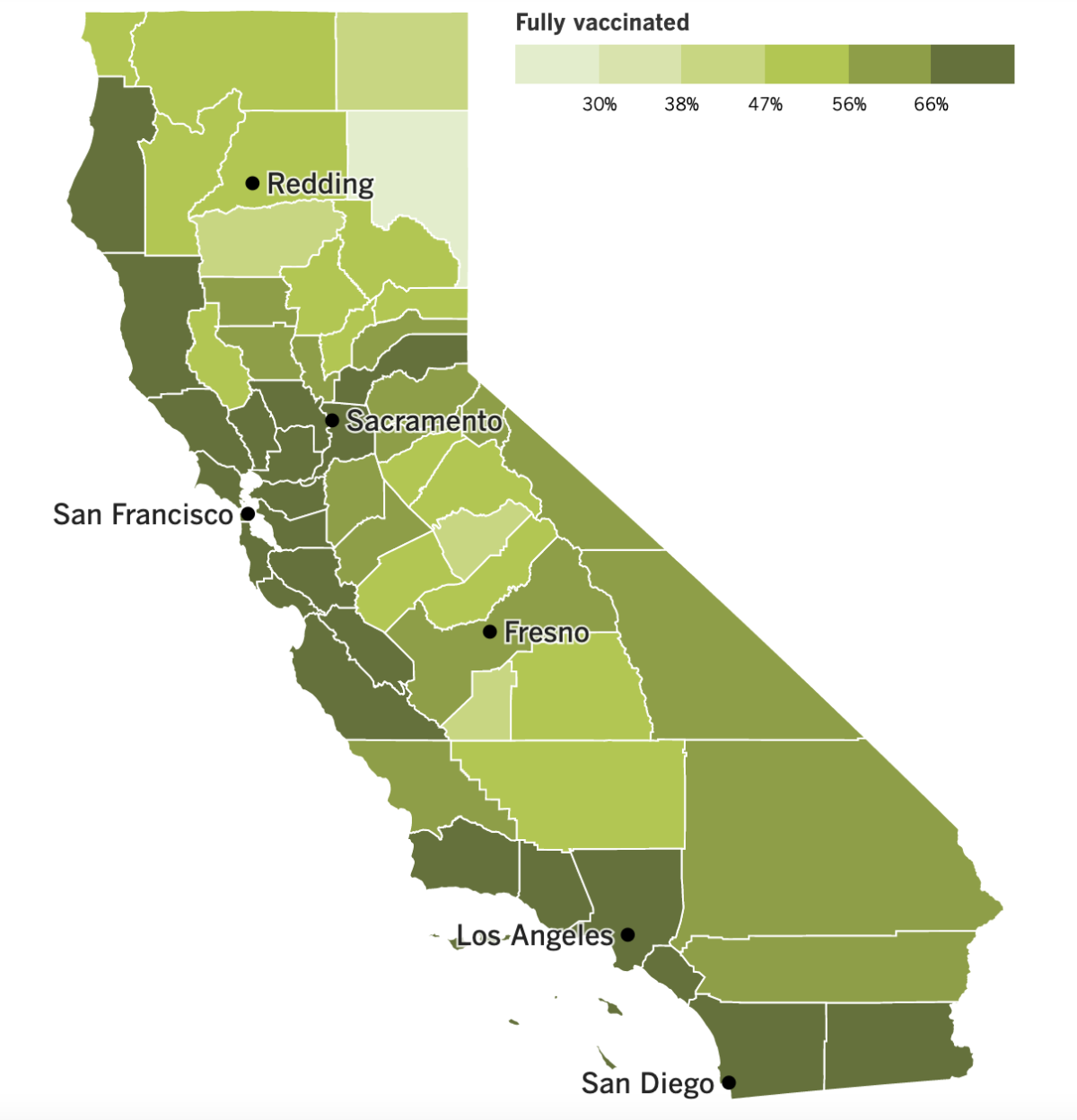
See the latest on California’s vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
As noted earlier, BA.5 is the big fish in the pond right now. People who managed to dodge the coronavirus before are getting caught in its clutches. The experts who track everything COVID are piecing together a picture of why this subvariant has, ahem, gone viral.
One reason is that the BA.5 strain is able to produce far more copies of itself than its predecessors. And it looks like it’s able to do that because it’s much more effective at getting inside of cells. That’s a key advantage, because once inside, it hijacks the cell’s machinery to pump out copies of itself. Those copies then go on to infect new cells.
This cycle “may help explain why this version of the virus has caused a lot of trouble, more than other Omicron subvariants,” Dr. Eric Topol, director of the Scripps Research Translational Institute in La Jolla, explained in a blog post.
Another factor is the speed with which new strains overtake older ones. Back in the day, variants like Alpha and Delta climbed to the top of the CDC’s Nowcast chart and stayed there for weeks or months. But in the 14 weeks represented in the chart right now, three distinct strains — BA.2, BA.2.12.1 and BA.5 — have all been dominant, with BA.5 rising the fastest.
With such rapid turnover, the immunity gained by an infection has a shorter shelf life. People who’ve been infected can be reinfected sooner. And many have been.
California reported about 10,400 coronavirus reinfections per week between mid-May and mid-June, a period when BA.5 and its close cousin BA.4 began circulating widely. For the sake of comparison, the state had about 2,300 weekly reinfections between early March and early May.
Overall, California had 278 official cases per 100,000 residents in the week that ended Thursday. That’s down more than 10% from the prior week, but reporting delays over the long Fourth of July weekend might explain the drop.
In Los Angeles County, the official case rate is up to 323 per 100,000 residents per week. (Both figures are surely lowballs, since the results of at-home tests aren’t always reported to health officials.)
More ominously, statewide hospitalizations of coronavirus-positive patients hit 4,277 Tuesday, the highest single-day total since late February. In L.A. County, the coronavirus-positive patient census was 1,153 as of Tuesday, up 54.4% in the past two weeks. The county is averaging 13 deaths per day over the past week — nearly double the rate from two weeks ago.
L.A. County Public Health Director Barbara Ferrer said it looks like we’ll once again have a “high” COVID-19 community level by the end of the month. The statistic that’s likely to seal our fate is the number of new coronavirus-positive patients admitted to county hospitals. Right now, the CDC says that number is 9.7 patients per 100,000 residents per week. That’s only slightly below the threshold of 10 patients per 100,000 per week.
However, Ferrer said the CDC combines hospitalization numbers for L.A. and Orange counties, and if you break them apart, you see that the actual figure in the O.C. is around 13, while the one for L.A. is 8.4. Given the discrepancy, Ferrer said she would use the county’s statistics to determine when L.A. has a high COVID-19 community level.
After that happens, if L.A. County remains in the “high” zone for two consecutive weeks, the indoor mask mandate will return, Ferrer said.
Masks are required at Malibu City Hall after four of the 85 people who work there became infected in the span of two weeks. Those infections qualified as a “worksite case cluster,” which prompted county health officials to impose a mask rule. It will remain in effect until at least two weeks after the last case.
A spokesman for Malibu said none of the infected people caught the coronavirus at work, nor did they spread it to coworkers.
With so many Americans coming down with COVID-19, the FDA announced a new policy last week that’s intended to make it easier to get a prescription for Paxlovid. Now pharmacists can prescribe the antiviral pill, which was previously available only from a doctor.
“Since Paxlovid must be taken within five days after symptoms begin, authorizing state-licensed pharmacists to prescribe Paxlovid could expand access to timely treatment,” said FDA drug center director Patrizia Cavazzoni.
In the early months of the pandemic, before there were COVID-specific medications, doctors frequently prescribed antibiotics to hospitalized COVID-19 patients. Antibiotics don’t treat viral infections, but the hope was that they would ward off bacterial infections that might hinder a patient’s recovery.
A new report from the CDC suggests that practice might have fueled a 15% increase in drug-resistant “superbug” infections in 2020. Prior to the pandemic, superbug infections had been on the decline, and deaths fell 18% between 2012 and 2017.
Antibiotic use dropped in 2021, and CDC experts expressed hope that when the data come in, they’ll see that the number of superbug infections followed suit.
And finally, a new version of Omicron has emerged in India, and scientists are concerned that its rapid growth and quick spread to other countries could make it the successor to BA.5.
The new subvariant, BA.2.75, appears able to dodge immunity from vaccines and past infections, just like its Omicron cousins. It’s too soon to say whether it makes people sicker.
At least three cases involving BA.2.75 have been identified in the U.S., including two on the West Coast.
“It’s still really early on for us to draw too many conclusions,” said Matthew Binnicker, director of clinical virology at the Mayo Clinic in Rochester, Minn. “But it does look like, especially in India, the rates of transmission are showing kind of that exponential increase.”
Your questions answered
Today’s question comes from readers who want to know: How can I protect myself against the super-contagious BA.5 subvariant?
Compared to other versions of the coronavirus — and even other versions of Omicron — BA.5 seems particularly difficult to evade. Its spike protein has changed enough that prior coronavirus infections don’t offer much in the immunity department, which explains why so many people are experiencing back-to-back illnesses.
COVID-19 vaccines are also less effective at blocking infections with BA.5, though they’re holding up when it comes to preventing severe illness and death.
“BA.5 is a different beast,” Dr. Robert Wachter, chair of UC San Francisco’s Department of Medicine, wrote on Twitter last week.
The virus might be different, but the measures you can take against it are the same as for other versions of SARS-CoV-2.
Get vaccinated and boosted. Staying up-to-date on your vaccinations is essential, especially considering evidence that being fully vaccinated but not boosted offers little protection against Omicron strains. Only 58% of Californians who completed their primary vaccination series have received their first booster shot, according to the state Department of Public Health. Nationwide, just 48% of Americans eligible for their first booster have received it.
Wear a mask. Face coverings are required in Los Angeles County if you’re on a bus, train, ride-share vehicle or other form of public transit. The same goes for transportation hubs like airports and train stations. For now, mask use is voluntary in most other settings statewide, but if you opt to wear one, it’ll be easier to keep BA.5 out of your airways. Bonus: You’ll be protecting the people around you too. Your best bet is a high-quality mask with a good seal around your nose and mouth.
Be careful at gatherings. If your summer just isn’t complete without barbecues and beach outings, there are things you can do to minimize your risk. Spending time outdoors is safer than being indoors. If you do go inside, wear a mask and make sure the space is well ventilated by opening doors and windows. Avoid dining indoors since you can’t eat with your mask on. Asking everyone to take a rapid coronavirus test before your gathering will make it less likely to become a superspreader event.
We want to hear from you. Email us your coronavirus questions, and we’ll do our best to answer them. Wondering if your question’s already been answered? Check out our archive here.
The pandemic in pictures

This is not a scene from a mass wedding of Moonies. The folks in the photo above were part of a do-over for couples whose marriage ceremonies became casualties of the COVID-19 pandemic.
Five hundred couples took part in the multicultural event Sunday at New York City’s Lincoln Center. The “weddings” weren’t legally binding, but they did feature bouquets, a procession, music, dancing and kissing — just like the real thing.
A reverend, an imam and a rabbi offered words of inspiration, and New York City Mayor Eric Adams addressed the happy couples. The hourlong ceremony ended with a unity ritual. Then the group reception got underway. It was a symbolic second chance to reclaim what the coronavirus had taken.
Resources
Need a vaccine? Here’s where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Here’s what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
We’ve answered hundreds of readers’ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




