What constitutes brain death? Depends on which hospital you’re in, study finds
When it comes to diagnosing brain death, policies that vary from hospital to hospital could open the door to unthinkable errors. Yet protocols designed to ensure that brain death gets diagnosed the right way every time have been adopted unevenly across the United States, new research shows.
In some cases, hospitals do not require doctors to follow protocols that would rule out conditions that mimic brain death but that can be improved with proper treatment. In other cases, hospitals adopted cumbersome procedures that delay the proper diagnosis of brain death, putting patients in need of donor organs at risk, according to a report published Monday in the journal JAMA Neurology.
Neurologists recognize that the doctors who are asked to make the crucial call for profoundly unresponsive patients are not always steeped in the diagnostic fine points of brain death, and they may lack the means to identify it with complete confidence. So in 2010, the American Academy of Neurology wrote a clear set of standards and procedures to distinguish a brain-dead patient from one who might emerge from an apparent coma.
The new report makes clear that many hospitals surveyed between 2012 and 2015 had not adopted these guidelines.
“This is disconcerting,” said David Magnus, a Stanford University medical ethicist who helped draft Stanford Health Care’s brain death protocols. The match between hospital rules and the American Academy of Neurology’s guidelines “should be 100%.”
In some states, any physician can make the diagnosis of brain death. Other states have laws that dictate the precise level of medical expertise such a doctor must have.
In addition, some states demand a confirmatory diagnosis by a second physician, or require a given period of time to elapse before brain death may be declared. Others do not.
Experts outlined several scenarios that show how this variability can lead to serious problems.
For instance, hypothermic patients who have been fished out of freezing water or snow may satisfy many of the criteria for brain death, but will often recover when warmed. Despite this, only 36% of hospitals surveyed said they required physicians to ensure a patient’s core body temperature reached near-normal levels before making a declaration of brain death.
Similarly, ingestion of certain drugs sometimes mimics the loss of primitive reflexes seen in those with no remaining brain activity. But only about 32% of hospitals surveyed required testing to rule out the possibility of toxic drug levels.
While an absence of spontaneous respiration is one clear criterion for diagnosing brain death, fewer than two-thirds of hospital protocols included detailed criteria for assessing that in an injured patient, the study found.
Other hospital protocols called for tests that have not been found useful in making a diagnosis of brain death. While conferring no greater certainty of brain death, these time-consuming extra steps can lessen the likelihood that a brain-dead patient’s organs would be donated to someone in need of a transplant.
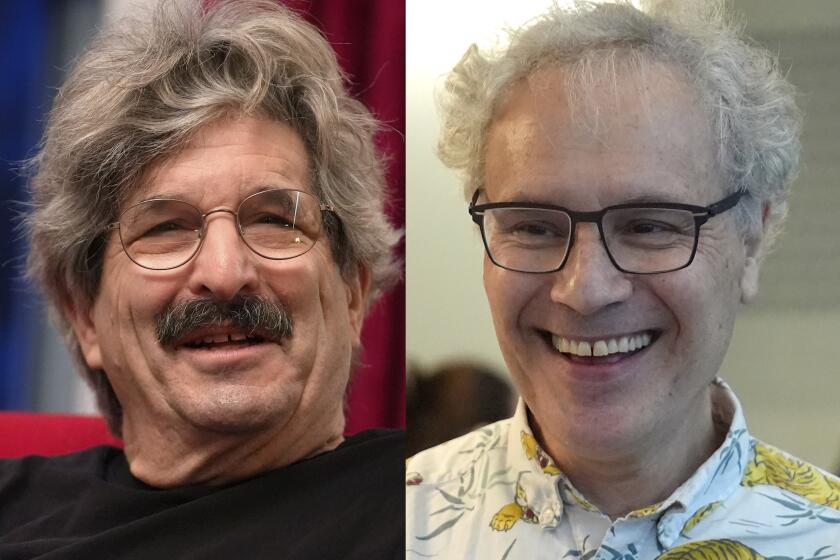
Martin Monti, a UCLA expert on coma and other disorders of consciousness, emphasized that when it comes to diagnosing brain death, “the science is there.” Given that unusual consensus, neurologists are right to “be pushy” and encourage hospitals to translate that science into practice every time.
Diagnosing someone as brain-dead when he or she is not would be a horrific error, Monti said. But measures that delay a correct diagnosis and reduce the availability of transplantable organs are also unacceptable, because they may deny a potential beneficiary a chance at life.
“This paper is a beautiful example of how good science and medicine and good practice go hand in hand,” Monti said. “The problem is that we really need to have an extremely uniform way of doing this because the devil really is in the details.”
Follow me on Twitter @LATMelissaHealy and “like” Los Angeles Times Science & Health on Facebook.