This retinal implant may one day cure blindness caused by macular degeneration

A look at the road leading to the first tests of a retinal implant designed to treat patients with a form of macular degeneration.
For many of the 10 million Americans who are losing their vision to a thievish eye condition with no treatment, help may be on its way.
In a very early clinical trial, researchers have implanted a stem cell “patch” to repair failing retinal cells in four patients with a condition called “dry” macular degeneration.
Three of the four patients who got the bioengineered implant — all of whom had lost their central field of vision and were legally blind — reported some lightening in the previously dark center of their visual field, according to a study published Wednesday in the journal Science Translational Medicine. The three also saw some improvement in their ability to see shapes and focus on letters or other objects directly in front of them.
In a span of roughly five months, one patient’s ability to identify letters on a vision chart improved by 17 characters.
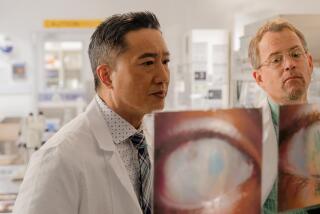
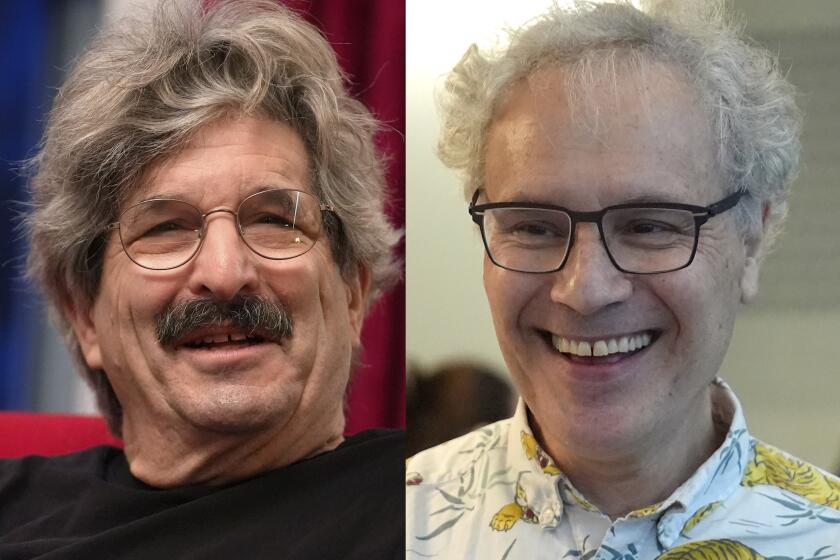
“It is remarkable when people can start seeing again,” said the study’s lead author, Dr. Amir H. Kashani of USC’s Roski Eye Institute at the Keck School of Medicine. Kashani conducted the trial with Dr. Mark S. Humayun, also a USC ophthalmologist, and a USC team that drew from many disciplines.
The modest improvements seen in this small group of patients offer hope in a field that has had nothing to offer patients yet, said Kashani, who is both an eye surgeon and stem cell scientist.
A treatment that would allow people with dry macular degeneration to look into the faces of loved one ”would be the dream,” Kashani said. “I don’t think we’re there yet.”
The experimental therapy drew from advances in a wide range of fields.
Researchers started with human embryonic stem cells, which are capable of giving rise to any type of human cell. In a lab, they coaxed those cells to become retinal pigment epithelium, or RPE, cells, which play a key role in keeping the retina healthy.
On a sterile sheet of inert polymer material much less than a hair’s breadth thick (6 microns to be exact), they grew a single layer of these RPE cells. Then they cut out patches smaller than a penny to implant inside patients’ eyes.
Finally, the team devised a special tool and a procedure to deliver a patch to the site of a patient’s failing RPE cells.
The researchers introduced the implant through a tiny incision in one eye’s outer periphery using a minuscule set of forceps. After creating a pocket between the retina and the failing RPE cells, they unfurled the patch — “like a soft taco,” according to one expert — inside the space and flattened the retina on top to hold it in place.
Close to 10 years in the making, the procedure was done on an outpatient basis, and subjects went home afterward.
Theoretically, embryonic stem cells have no individual signature of ownership that might prompt an immune system attack, and a healthy eye is normally sealed off from the immune system anyway. But to ward off a possible immune response to the transplanted tissue, the experimental subjects got a low dose of anti-rejection drugs for six to seven weeks.
In followup periods that lasted four to 12 months, the researchers watched as the implants’ stem cells stayed put and successfully integrated with the patients’ own retinal tissue. The anatomical changes in these retinas suggested that the failing RPE cells that cause dry macular degeneration had sprung back to life and were beginning to work again.
The trial was primarily designed to test the safety of the potential therapy. However, the researchers were able to see some signs of improved visual function.
Kapil Bharti, a molecular biologist at the National Eye Institute in Bethesda, Md., who is working to bring a slightly different stem cell treatment for macular degeneration to trial, hailed the preliminary report as a “first of its kind” use of stem cells and bioengineering for the condition.
Bharti, who was not involved in the new study, called it a key step on the road to a treatment for dry macular degeneration and a milestone for regenerative medicine.
As “the first tissue-engineered product” to be tried on this form of blindness, its preliminary record of safety is a “remarkable” achievement, he said.
At the same time, he acknowledged that it could take years to establish the safety, effectiveness and technical and commercial viability of a stem cell treatment like this one.
Bharti hopes to begin human trials at the National Eye Institute this year on a similar stem cell patch for the dry form of macular degeneration. Instead of using embryonic cells, Bharti’s team is working with induced pluripotent stem cells — mature cells that are harvested from a patient and then “reprogrammed” back to a primitive phase in which they could give rise to many different kinds of tissue.
Last month, a British research team reported that it had used an experimental stem cell therapy to improve visual acuity in two subjects with the “wet” form of macular degeneration, in which the failure of the RPE cells causes vessels in the eye to break and become leaky.
Future trials of the USC team’s therapy will be conducted on subjects with less advanced disease, and they may well show more dramatic effects in halting or reversing the progressive vision loss that is a hallmark of dry macular degeneration, both Bharti and the team members said.
The therapy is designed to rescue RPE cells which typically die off over many years. So it is likely to work best in patients whose cells are at least partially intact. As the therapy is tried on patients whose disease is not so far along, Bharti said he was “cautiously optimistic” that evidence of its effectiveness will grow.
Currently, about 10 million Americans are thought to suffer from dry macular degeneration. Because it progresses very slowly, roughly 8 in 10 sufferers have vision that is partially or slightly impaired, particularly in the central field. The brain can compensate for a while, but eventually patients lose all but the most peripheral vision.
Anna Keuhl, a retired accountant in Palos Verdes, may offer a glimpse of the therapy’s effects on patients with disease that is less advanced. Now 78, she has a family history of dry macular degeneration, and first detected its earliest signs — a scarcely perceptible loss of central vision — just over 20 years ago.
Keuhl is not yet legally blind. But she has given up on driving, and she relies on her husband to make sure her t’s are crossed and her umlauts are in place in handwritten letters to friends in her native Germany.
During hikes in Palos Verdes last spring, she could still see the mariposa lilies in her peripheral vision. But when she bent down to focus on their velvety interiors, she would lose them in a widening spot that had gone gray.
Keuhl is part of the second wave of patients getting the experimental treatment in the lab of Kashani and Humayun. Since receiving her stem cell implant last October, “I notice little things,” she said. While watching TV, she can focus on faces better and follow plots that require distinguishing one character from another. She is better able to look, full-on, at her face in the mirror and apply makeup.
And this spring, as the mariposa lilies begin to bloom, “I’ll see those details,” she said.
“I don’t know how far this is going to go, how many cells are going to return,” she added. “We’ll see.”
MORE IN SCIENCE
If two eyes are good, four were even better for this lizard species
A sudden loss of wealth may be hazardous to your health
Bringing meals to people with food insecurity may deliver savings to the healthcare system