How the coronavirus will change your next dentist appointment
Surgical masks are replaced with N-95 respirators, the dental drill is silent, and waiting-room magazines are gone. Your next trip to the dentist may be much different from what you’re used to.
Four decades after the AIDS epidemic changed dentistry, requiring providers to wear gloves and goggles for the first time, the novel coronavirus is challenging the industry again to step up its sanitizing standards as patients begin to return for routine care amid a global pandemic.
“Dentists are really great at infection control and being prepared to create safety,” said California Dental Assn. President Richard Nagy, a periodontist in Santa Barbara. “That’s what we’re good at, and that’s what we’re doing.”
Although the Occupational Safety and Health Administration deems dentistry “very high risk” for coronavirus transmission, there have been no COVID-19 clusters linked to dental settings or among dental healthcare professionals, according to the CDC. But in March as the pandemic began to escalate in the U.S., most offices were limited to just handling emergencies. To set a “new normal” as patients return, the CDC and the California Department of Public Health issued guidance on May 3 and 7, respectively, revamping the routine, including pre-care screenings, which tools to use and how air is filtered inside offices.
Here’s what the recommendations mean for your next dentist appointment:
Why dentistry needs extra precautions
The coronavirus is known to spread through respiratory droplets emitted when an infected person sneezes, coughs or talks. However, many standard dental procedures that require ultrasonic instruments can aerosolize the virus by creating a spray containing a mix of water, saliva and other debris, according to the CDC. When the coronavirus becomes aerosolized, the large droplets that quickly fall to the floor or other surfaces instead can hang in the air for longer periods of time.
Due to the risk of aerosolizing the virus, the CDC is emphasizing properly maintained ventilation systems as dental offices reopen. In addition to opening windows to promote air circulation when possible, the CDC recommends that offices consider using portable HEPA air filters during and following aerosol-generating procedures. The filters reduce particle count and turn the air in the room over faster.
For any aerosolized particles that aren’t filtered out during a procedure, the CDC recommends that employees wait 15 minutes after a patient leaves the treatment room before disinfecting the room’s surfaces. This allows droplets, even those hanging in the air, to fall and be cleaned through the dental office’s standard protocols.
What to expect before sitting in the dentist’s chair
The coronavirus changes could start days before your dentist appointment, as the CDC and state authorities advise pre-screening of patients through phone calls prior to receiving care. Dental offices are calling patients to ask about any symptoms of possible infection within the past two to 14 days and any contact with COVID-19-positive people. When patients arrive at the dentist’s office, they are screened again with the same questions and get their temperature taken. Anyone suspected of having an active COVID-19 infection should not be seen for dental care.
Masks are required at all times inside the office for employees and patients, except while they are receiving care, and the California Department of Public Health encourages dental offices to have a supply of face masks to give to patients who do not have their own.
The CDC also recommends that chairs in waiting rooms be placed at least six feet apart for social distancing, and that appointments be staggered to prevent patients from congregating in the waiting room.
Patients can call their dentists and ask how they are complying with the CDC recommendations or even come in to see the office before scheduling an appointment.
What to expect during the exam
Because of the risk of aerosolizing the virus, the official recommendations are to limit use of certain dental tools. Anything like ultrasonic drills, polishing tools and the air/water syringe that could mix water with the saliva in a patient’s open mouth are to be avoided, if possible.
For those returning to the dentist for a regular cleaning, that means hygienists will likely just use hand tools instead of the ultrasonic scaler or a combination of the two. Using hand tools exclusively may take longer, but it’s just as effective, said Natasha Lee, a private practice dentist in San Francisco who was included on Gov. Gavin Newsom’s business and jobs recovery task force.
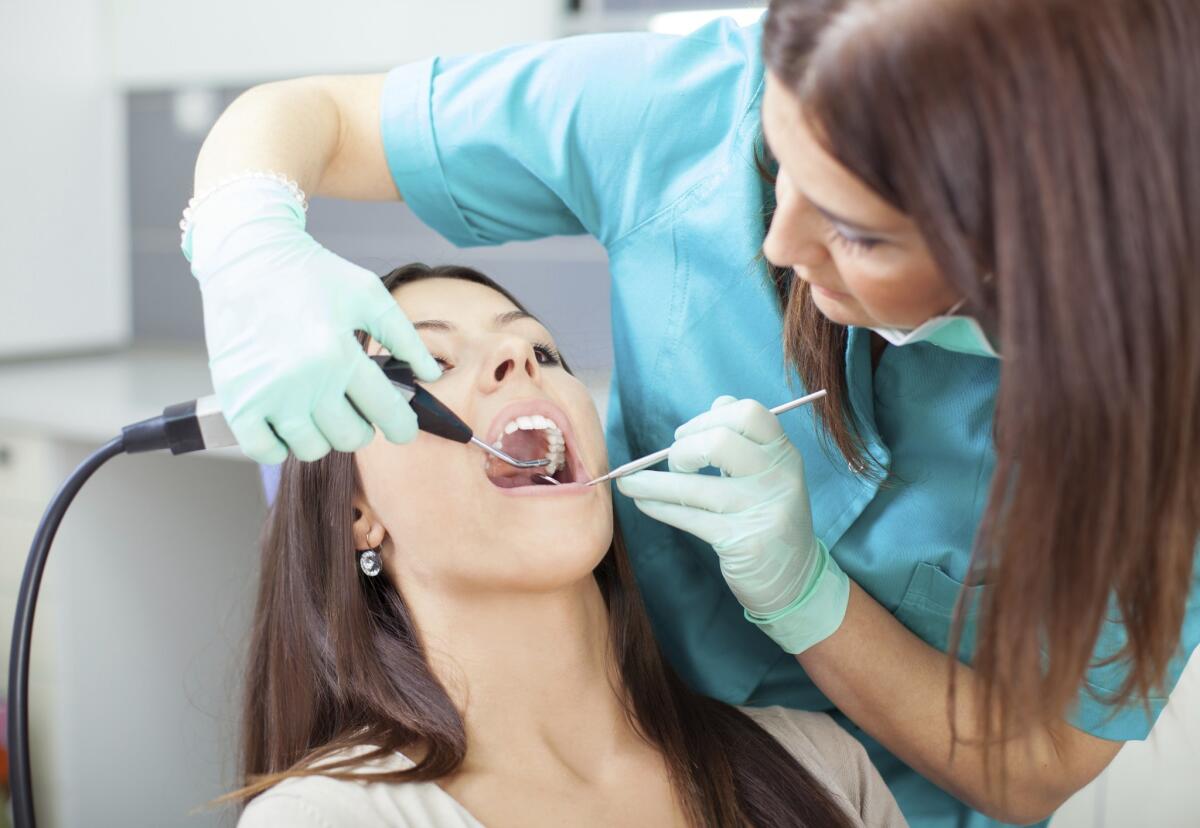
For other procedures that require the use of ultrasonic tools, dentists are advised to use a rubber dam to isolate the tooth and employ four-handed dentistry. The dentist, outfitted with all necessary personal protective equipment including an N-95 mask, will perform the procedure while a similarly protected dental assistant or hygienist will be at the patient’s side holding a high-evacuation suction device. The large white straw has an ability to suction away 90% to 95% of the water spray coming from a patient’s mouth, Lee said.
Considering all the precautions, from screening before the appointment to the layers of protection during treatment, “we feel like dentistry is one of the safer places that you could be,” Lee said.







