COVID-19 vaccines may not work on nursing home patients. Is it worth the risk to try anyway?

The roughly 3 million Americans who reside in nursing homes, assisted living facilities and other group-care communities are an almost invisible population.
This week, however, they were singled out for high-priority access to a most precious resource: some of the first doses of COVID-19 vaccine available in the United States.
It’s a distinction they’ll share with the nation’s 21 million healthcare workers, thanks to a vote by the Advisory Committee on Immunization Practices, an expert panel that advises the federal Centers for Disease Control and Prevention.
In some eight months of debate among the 14 members of ACIP, the idea of prioritizing healthcare workers was never in doubt. The ability of these doctors, nurses, pharmacists, paramedics, hospital staffers, medical technicians and home health aides to show up for work is essential to our weathering the pandemic.
They are widely hailed as heroes, running toward danger while those who can protect themselves do so by staying home. Their jobs caring for the sick have led to outsize rates of infection and severe illness in their ranks — though they make up about 6% of the country’s population, they account for 12% of U.S. COVID-19 cases.
It’s a profile starkly different than that of patients who live in long-term care facilities. Retired from active life, they are on the receiving end of medical care. Indeed, they are so medically fragile that some fear the vaccine itself could hasten their demise.
If vaccines for diseases like the flu are any guide, the new COVID-19 shots may not be particularly effective in nursing home residents. The aging immune system is notoriously difficult to rouse with vaccines.
Federal regulators will consider requests in December by Pfizer and Moderna for emergency use authorization for their coronavirus vaccines.
Neither of the first two COVID-19 vaccines likely to win emergency use authorization from the Food and Drug Administration — one from the pharmaceutical giant Pfizer and the other from a start-up named Moderna — has been studied in the kinds of very elderly, very frail patients who populate long-term care facilities. (In clinical trials largely involving thousands of younger, healthier adults, they’ve been shown to be more than 90% effective.)
Yet if states opt to follow ACIP’s advice, this group will get the scarce vaccine before teachers, before workers deemed essential to the economy, and before younger seniors and those with underlying conditions.
Why?
Put simply, they have paid for the privilege with their lives.
More than 100,000 long-term care residents have died from COVID-19 in the U.S. And though patients in these facilities make up less than 1% of the U.S. population, they account for 7% of the nation’s coronavirus caseload and 40% of its COVID-19 deaths.
That death toll is likely to mount in the coming weeks. By mid-November, more than 16,000 coronavirus infections were reported in nursing homes and assisted-living centers, according to a report by the American Health Care Assn. and the National Center for Assisted Living. Nursing homes are now experiencing the worst outbreak of new cases since the spring, with more than 2,000 residents succumbing to the virus each week, said Mark Parkinson, who leads the combined group.
“The mortality rate is massively different” from that of the general population, said Dr. Helen “Keipp” Talbot of Vanderbilt University, who studies vaccine effectiveness in the elderly. “It’s not a little different. It’s completely different. That’s what drove those residents ahead of everyone” in gaining access to scarce doses of vaccine, she said.
COVID-19 vaccines: Healthcare workers and residents of long-term care facilities should be at the front of the line, a government advisory panel says.
In Tuesday’s 13-1 ACIP vote, Talbot was the only one who objected to prioritizing long-term care residents. She dissented, she said, to send a message that the oldest and most vulnerable must not be an afterthought in the development and testing of vaccines they are likely to need.
“I had to make a little bit of a stand,” Talbot said.
“It’s not because I hate Grandma — I love Grandma!” she added. “But we need to think about this population, plan for them and protect them.”
Virtually the definition of a vulnerable population, those residing in long-term care facilities need basic assistance and skilled medical care just to live. To secure it, they’re often sequestered in group settings that make social distancing — one of the few protections against coronavirus infection — nearly impossible.
They may seem cut off from the world, but they are far from protected. Their facilities are staffed by armies of low-wage workers who are among the most likely to become seriously ill with COVID-19. Black and Latino Americans — populations in which the disease has taken a disproportionate toll — make up 40% of their ranks.
In 2018, half of nursing assistants — who help residents bathe, feed and care for themselves — earned less than $13.38 per hour. Paid sick days are a rarity, and many go home to crowded, multi-generational living conditions where coronavirus infections have seen intense levels of spread.
When people talk about COVID-19 vaccines, they can sound like they’re speaking a foreign language. Don’t worry! Here’s your guide to vaccine vocabulary.
The socioeconomic circumstances of these workers also mean they’re more likely to suffer from many of the underlying conditions that raise the risk of severe COVID-19, including asthma, obesity and diabetes.
For the medically fragile residents of long-term care facilities, the implications are stark.
“Long-term care facilities are powerless to fully prevent [the coronavirus] from entering due to its asymptomatic and pre-symptomatic spread,” Parkinson said. As the virus runs rampant among the general population, “our worst fears have come true.”
Residents are suffering the most, even though they’re clearly not to blame, Talbot said.
“If you are in a facility and cannot leave, you are not bringing virus into that facility,” she said. “It’s only the people that work there that bring those viruses with them — from church, home, restaurants, grocery stores.”
That has made the vaccination of those who staff long-term care facilities a key aim. Not only will it protect a key segment of healthcare workers, it will also indirectly protect the people they care for.
There are still many unknowns when it comes to the pandemic, but the early signs of success for two experimental COVID-19 vaccines make a few things clear.
Doesn’t it make sense to vaccinate residents at the same time, even if the data on its safety and effectiveness are scant?
Several members of ACIP said they believe it does.
“You’re coming through and vaccinating staff and you’ve got people who can benefit,” said Dr. Paul Hunter, a University of Wisconsin family medicine specialist. Those in nursing homes and residential care might not get another convenient chance to be vaccinated.
“It’s an efficiency” to vaccinate both at the same time, he said.
Doing so, however, will come with an obligation to explain to the residents, their families and their doctors that the vaccines come with substantial uncertainty for elderly and frail people, who were not included in clinical trials.
It’s possible that the vaccine may not work. On the other hand, it could provoke a strong immune response that leaves patients feeling lousy for days.
“We don’t know all that information, and in an ideal circumstance we would not make recommendations without it,” said Dr. Robert Atmar, an infectious disease specialist at Baylor College of Medicine and ACIP member. “But we’re not in an ideal circumstance. We’re in the middle of a raging epidemic, and lot of us were moved by the suffering we’ve seen in long-term care facilities over the past eight months.”
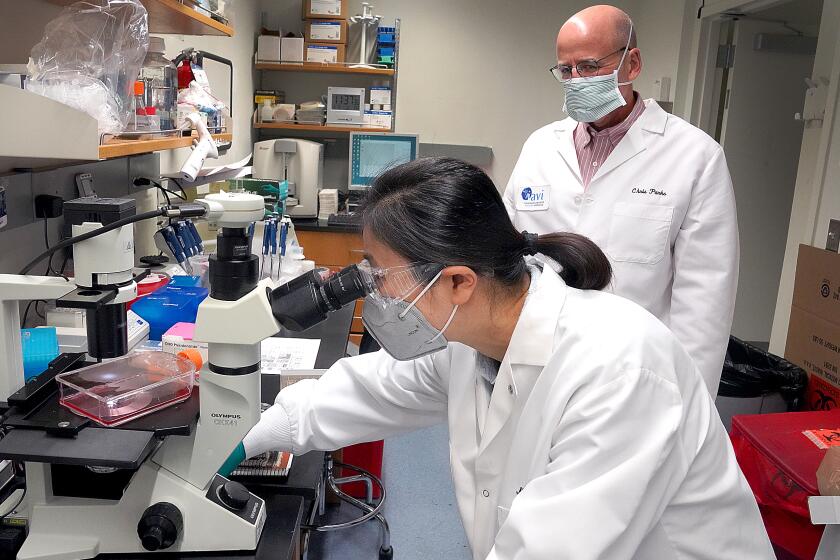
A small lab tries to alter one gene of the coronavirus, hoping that change will offer a way to kill it.
Atmar said he is not so concerned that the vaccine itself will prove unsafe, but that some nursing home residents’ mild reactions could prompt medical workups, hospitalizations and treatments that are risky and unnecessary.
The CDC assured ACIP members it would draft fact sheets to help guide residents and their caregivers in making their decisions. But with so many unknowns, it may not be enough, Talbot said.
If a loved one dies after receiving a vaccine, will families feel responsible? Will they blame the vaccine and refuse to take it themselves?
Furthermore, will the inevitable reports of post-vaccination deaths — many of which will be due to unrelated causes — undermine the public’s shaky confidence in the vaccine’s safety, as some experts fear?
With little science to answer the last question, experts said they had little choice but to put this hard-hit population at the front of the line and hope the COVID-19 vaccine helps, at least a little.
“It won’t necessarily be the home run that we want,” Talbot said. “But it’ll probably be a good solid base hit.”