What we’ve learned from the nearly 1 million who’ve died of COVID-19
The nearly 1 million people around the world who have lost their lives to COVID-19 have left us a gift: Through desperate efforts to save their lives, scientists now better understand how to treat and prevent the disease — and millions of others may survive.
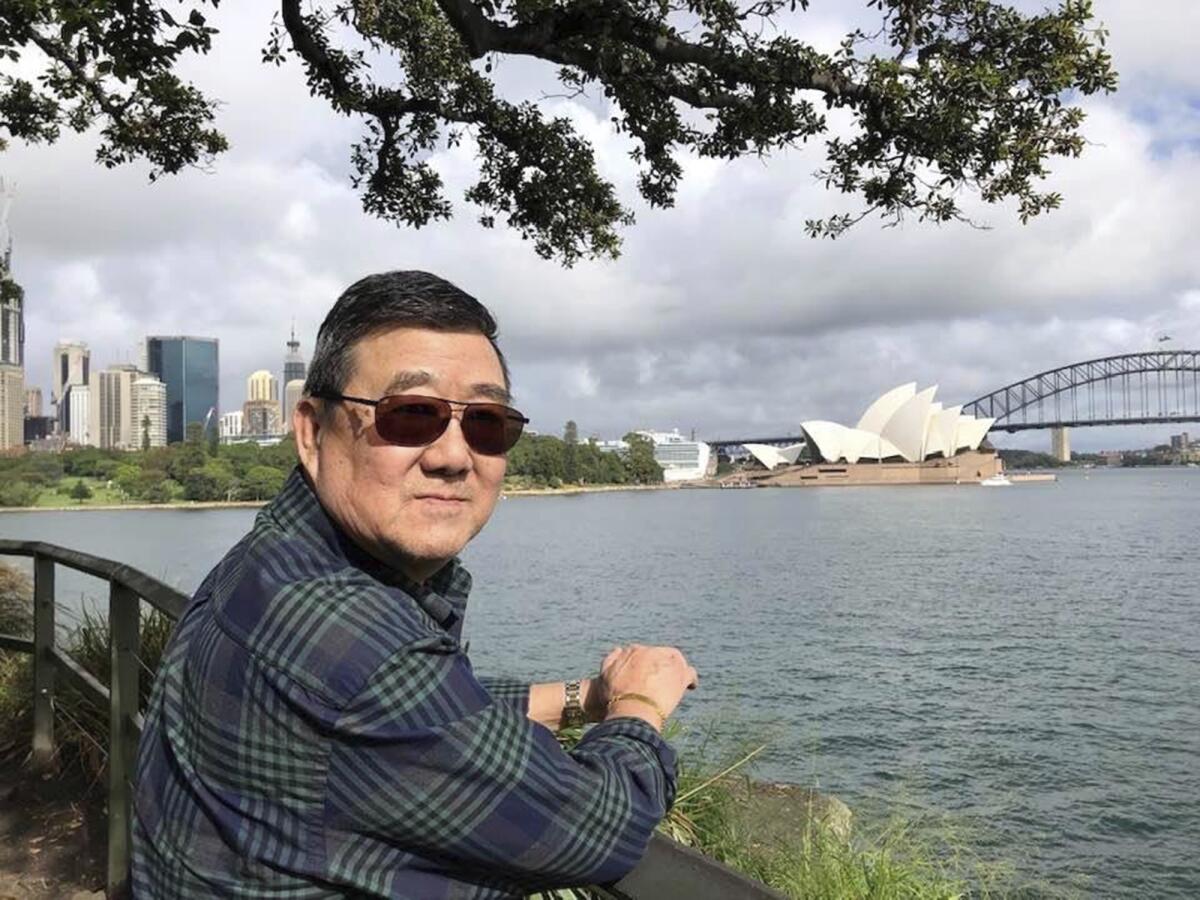
Ming Wang, 71, and his wife were on a cruise from Australia, taking a break after decades of running the family’s Chinese restaurant in Papillion, Neb., when he was infected. In the 74 days he was hospitalized before his death in June, doctors frantically tried various experimental approaches, including enrolling him in a study of an antiviral drug that ultimately showed promise.
“It was just touch and go. Everything they wanted to try we said yes, do it,” said Wang’s daughter, Anne Peterson. “We would give anything to have him back, but if what we and he went through would help future patients, that’s what we want.”
Patients are already benefiting. Though more deaths are expected this fall because of the recent surge in coronavirus infections in the U.S. and elsewhere, there also are signs that death rates are declining and that people who get the virus now are faring better than did those in the early months of the pandemic.
Even with California’s death toll from COVID-19 surpassing 10,000, some hope is emerging: Doctors are getting better at saving patients.
“Some of the reason we’re doing better is because of the advances,” said Dr. Francis Collins, director of the U.S. National Institutes of Health. Several drugs have proved useful and doctors know more about how to care for the sickest patients in hospitals, he said.
We’re in the “stormy adolescence” phase of learning what treatments work — beyond infancy but not “all grown up either,” Collins said.
The nearly 1 million deaths attributed to the coronavirus in nine months are far more than the 690,000 from AIDS or the 400,000 from malaria in all of 2019. They’re trending just behind the 1.5 million from tuberculosis.
Wealth and power have not shielded rich countries from the awful power of the virus. The United States “has been the worst-hit country in the world” with more than 7 million coronavirus infections and more than 200,000 deaths, reflecting “the lack of success that we have had in containing this outbreak,” Dr. Anthony Fauci, the nation’s top infectious disease specialist, told a Harvard Medical School audience this month.
More than 40% of U.S. adults are at risk for severe disease from the virus because of high blood pressure and other conditions. It’s not just old people in nursing homes who are dying, Fauci stressed.
Dr. Jesse Goodman, a former U.S. Food and Drug Administration chief scientist now at Georgetown University, agreed.
“Nobody should make a mistake about this” and think they’re not at risk just because they may not personally know someone who has died or haven’t witnessed what the virus can do firsthand, he said.
The older you are, the greater your risk for a severe case of COVID-19, the CDC says as it expands its list of risky underlying health conditions.
Although cases are rising, death rates seem to be falling, said Dr. Cyrus Shahpar, a former U.S. Centers for Disease Control and Prevention scientist now at the nonprofit group Resolve to Save Lives.
The virus’ true lethality — the infection fatality rate — isn’t yet known, because scientists don’t know how many people have been infected without showing symptoms.
What’s often reported are case fatality rates — the portion of people who have tested positive and then gone on to die. Comparing these from country to country is problematic because of differences in testing and vulnerable populations. Tracking these within a country over time also carries that risk, but it can suggest some trends.
“The U.S. cumulative case fatality rate in April was around 5%. Now we’re around 3%,” Shahpar said.
In England, researchers reported that case fatality rates have fallen substantially since peaking in April. The rate in August was around 1.5% versus more than 6% six weeks earlier.
One reason is changing demographics: More cases these days are in younger people who are less likely to die from their infection than older people are.
The median age of people with COVID-19 in the U.S. has declined, with adults in their 20s now accounting for more cases than people in any other age group.
Increased testing also is playing a role: As more people with mild or no symptoms are detected, it expands the number of known infections and shrinks the proportion that prove fatal, Shahpar said.
It’s clear that treatments also are affecting survival, many doctors said. People who have died from COVID-19, especially ones who took part in studies, have helped reveal what drugs do or do not help.
Dexamethasone and similar steroids now are known to improve survival when used in hospitalized patients who need extra oxygen, but might be harmful for less sick patients.
An antiviral drug, remdesivir, can speed recovery for severely ill patients, shaving four days off the average hospital stay. Two anti-inflammatory drugs, one used in combination with remdesivir — the drug Wang helped test — also have been reported to help, although results of those studies have not yet been published.
The jury is still out on convalescent plasma, which involves using antibody-rich blood from survivors to treat others. No large, high-quality studies have tested this well enough to know if it works.
The value of rigorous, scientific studies to test treatments has become clear, Goodman said. “We certainly see what happens” when treatments are widely adopted without them as hydroxychloroquine was, he said. “That exposed a lot of people to a potentially toxic drug” and delayed the hunt for effective ones.
Aside from drugs, “the case fatality rate is actually improving over time as physicians get more adept at taking care of these very sick patients,” said Dr. Gary Gibbons, director of the U.S. National Heart, Lung and Blood Institute.
In hospitals, doctors know more now about ways to avoid using breathing machines, such as keeping patients on their bellies.
“We’ve learned about how to position patients, how to use oxygen, how to manage fluids,” and hospitals have increased their surge capacity and supplies, Dr. Judith Currier, a UCLA physician, said at a recent webinar organized by the American Public Health Assn. and the U.S. National Academy of Medicine.
The coronavirus crisis has upended the status quo in all kinds of ways, and that includes how clinical trials are run.
The best way to avoid dying from the coronavirus remains to avoid getting it, and experience has shown that the simple measures advocated by public health officials work.
“Prevention is the most important step right now as we’re waiting for a vaccine and we’re improving treatment,” Goodman said.
Wearing a face mask, washing hands, keeping at least 6 feet apart and disinfecting surfaces “clearly are having a positive effect” on curbing spread, Fauci said.
If more people stick with common-sense measures like closing bars, “we should improve our ability to manage this” and prevent more deaths, Shahpar said. “It should take longer to get to the next million if it ever happens.”










