The loneliness of being immunocompromised in the age of COVID-19
This story was originally published in Group Therapy, a weekly newsletter answering questions sent by readers about what’s been weighing on their hearts and minds. Sign up here to get it in your inbox.
When the bustle of New York City abruptly halted, giving way to empty streets and overflowing hospitals, Una Aya Osato was very sick.
It was March 2020, and Osato didn’t know that the effects of COVID-19 would morph into a chronic illness now known as long COVID. It was an awful time for Osato, her city and the world at large, but there was this feeling of everyone being in this together, even though the pandemic affected each person differently.
Get Group Therapy
Life is stressful. Our weekly mental wellness newsletter can help.
You may occasionally receive promotional content from the Los Angeles Times.
“We were all so connected. Not only were we connected because this virus spread through each other and in the air we breathe, we had to be connected in order to get through this,” said Osato, a performer, sex educator and disability justice advocate. “We needed each other.”
That unlikely state of togetherness did not last long. Most of us emerged the next year eager to get on with our lives. Some chose not to get vaccinated. Many stopped wearing masks in public places. And that left people who are immunocompromised, disabled or elderly fending for their own safety.
For Osato, this has meant opting out of what they once knew as a “normal life.” No one is masked in the venues where she once performed burlesque, and as a result, they don’t feel safe doing that work in those settings. The same goes for public high schools, where they teach sex ed. “All these communities I was a big part of, I’ve had to make choices for my health to not be part of them,” Osato told me. “I feel like we’re all living in different worlds, parallel universes.”
We’ve received a few emails from Group Therapy readers that echo this sense of isolation and otherness:
“I have autoimmune issues, and I’m not able to go out without a mask and super caution. I feel left behind by the rest of the public moving on with their normal lives without masks. It’s like my illness is making me pay twice!”
“I’d like some mechanisms for isolation issues to someone moving into their senior years and finding that COVID only intensified the issues with feelings of abandonment; loss of parents; no nearby relatives, and being an older single in L.A.”
For those of us lucky enough to have immune systems more likely to protect us from the worst outcomes of COVID-19 — myself included — we’ve willfully denied the realities of immunocompromised people by acting in ways that ignore their needs. I have been guilty of going into grocery stores, music venues and restaurants unmasked in recent months. The process of reporting this newsletter has made me think twice about how I’ve chosen to “move on.” My editor and I respectfully admit that mentality has shown in our newsletter. We were reminded when a reader wrote to us after one COVID-themed newsletter reminding us: “You should not speak of the COVID pandemic as if it’s a past event. The best experts say it is still with us.”
In this piece, though, I also want to speak directly to those that we, the collective, have been doing a poor job considering and protecting. I’ll let Osato start us out.
“I really want to affirm to the people who wrote these emails that there are so many of us out here who feel that way,” they said. “It’s so lonely to know that our most vulnerable don’t feel safe going outside, and that’s not a priority for other people.”
The weight of loneliness
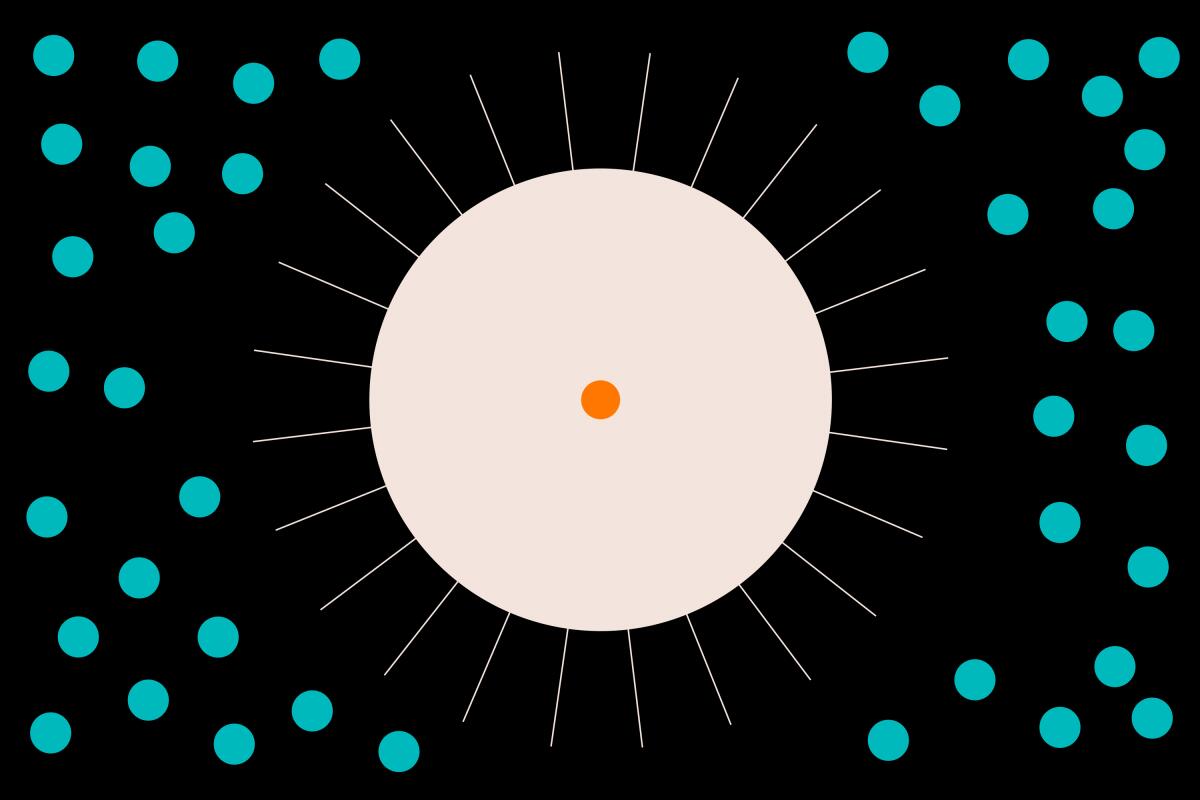
The feeling that is threaded throughout the complex experiences of Osato and other immunocompromised people in recent years is that of loneliness.
Columbia University researchers define loneliness as “the subjective feeling of inadequate meaningful connection to others.” In other words, it’s “a gap between the level of connectedness that you want and what you have,” one New York Times writer elegantly put it. It is different from social isolation, which is measured by the number of one’s social contacts. It is a subjective feeling.
Loneliness has become pervasive globally, so much so that in recent years it has been named as a serious public health concern, even an epidemic. In 2019, before COVID, 61% of Americans older than 18 reported that they were lonely. Rates were as low as 11% in the 1970s.
Researchers have cited several causes for this alarming shift: changes in family structure and the increase in people living far from relatives, a capitalistic culture that encourages independence and isolation, the weakening of local institutions that have historically fostered intergenerational relationships, and social media.
Loneliness is part of being human, an evolutionary alarm system that tells us we need to connect with others for the sake of our survival, said Ami Rokach, a professor of clinical psychology and expert in loneliness at York University in Canada.
When loneliness is with us for a long time, it increases the risk of depression, anxiety and substance use disorders, as well as heart disease, cancer, stroke, hypertension and dementia.
“To me, the most pronounced way loneliness can affect physical health is through immune suppression,” said Kory Floyd, professor of communication and psychology at the University of Arizona. “When you’re chronically lonely, you’re more likely to get sick, and your body may take longer to recover from illness or injury.”
All of that to say, it is no small thing to be continuously lonely. Not everyone who is immunocompromised in the age of COVID-19 is lonely, but our culture has created the conditions for that to be more likely — and as Floyd pointed out, loneliness puts them at an even higher risk for illness.
“In North America, we are a culture writ large that values individuality and autonomy, the idea that you can be anything you want to be if you just work hard enough,” Floyd said.
But this incessant drive to achieve often comes at the cost of community. Caring for our neighbors is not in service of climbing the socioeconomic ladder — or for many people, just surviving in a country with immense income inequality — so it falls to the bottom of our to-do lists, a footnote in the social contract.
So what can we do?
I asked this week’s sources what we can do to collectively confront the isolation and loneliness that the immunocompromised, the disabled, and our elders are experiencing because of COVID-19 and our response to it.
Check in with the people around you: It’s likely that you have at least a handful of people in your life who must take extra precautions to prevent themselves from contracting COVID-19, or from passing it on to a vulnerable loved one. Check in with them regularly, Osato said.
“Think about how you can help them feel safe and connected,” they said. “Sit on a bench with them outside, call them, text them, send them letters and videos. I think people just want to know they’re not forgotten.”
- Minimize spread: Over the past year or so it’s become the norm, even in California, to not wear a mask in public spaces. But we can easily reduce transmission by masking up indoors and staying at home when we’re sick, when we can. The peer pressure to not wear a mask is strong, but doing so is a simple act that also indicates empathy and helps high-risk people feel less alone in their experience, said Louise Lerminiaux, a patient advocate consultant who has spent the pandemic protecting herself and the kidney she was gifted 14 years ago.
- Listen to and support the demands of disability justice advocates, who are calling for more robust funding and research into understanding chronic illnesses and disabilities, and expanded government assistance for disabled people, Osato said. People with disabilities are more than twice as likely to live in poverty than non-disabled people, and barriers to accessing the social safety net (like the onerous process of applying for Social Security disability benefits) make it much harder for them to escape poverty.
I asked Osato what advice she would give to people who are in the position that she’s been in for the past three years. Here is what they said:
“Some things I’ve learned about being sick I’ve also applied to loneliness — how I care for my body through sickness and in loneliness.
“I’m gentle with myself as much as possible. I go slow, so slow that I can actually hear what my body needs. I deepen my learning and connection with people who are doing disability justice work. When you feel lonely, there’s something so grounding about knowing you’re a part of something bigger. The world is so broken, there’s infinite places to be part of social change.
“I seek wisdom and comfort from nature. I try to find joy in places that might surprise me. I journal, I draw. I listen to what I’m learning through what is such a painful and unfair process.
“And I know I’m not alone in my pain and loneliness. There have been so many before us, there are so many now, and there will be more of us in the future. Holding that pain and joy of being alive is part of all of our journeys.”
Until next time,
Laura
If what you learned today from these experts spoke to you or you’d like to tell us about your own experiences, please email us and let us know if it is OK to share your thoughts with the larger Group Therapy community. The email [email protected] gets right to our team. As always, find us on Instagram at @latimesforyourmind, where we’ll continue this conversation.
See previous editions here. To view this newsletter in your browser, click here.
Enjoying this newsletter? Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
More perspectives on today’s topic & other resources
Almost three years into the pandemic, many Americans have decided that the health emergency is over. But for patients whose immunity is weakened or destroyed by medicines or disease, it’s actually taken a turn for the worse, reports my colleague Melissa Healy. Two therapies that have been a mainstay of protection for these patients are no longer believed to be effective against two of the most dominant subvariants of Omicron, leaving them with only two effective medications should they get sick.
What does society owe immunocompromised people? They have always lived with a higher risk of infection, but COVID represents a threat that, for many, has further jeopardized their ability to be part of the world. Whether that changes depends on the accommodations society is willing to make, writes Ed Yong of the Atlantic. “Exactly none of the people I talked with wants a permanent lockdown,” Yong noted.
“The Long COVID Survival Guide” provides support for those who find themselves in the uncharted territory of this new illness, including how to get diagnosed, confronting medical racism, navigating employment issues, dealing with fatigue and neurological symptoms, and caring for your mental health. More than 20 experts contributed to this book.
Other interesting stuff
In the news and on social media, we hear the term “bipolar disorder” a lot, but misconceptions about the condition are rampant. My colleague Karen Garcia spoke with mental health experts about what bipolar disorder actually is, the push for thinking about the condition as one that’s on a spectrum, and the stigma that can come with a diagnosis.
Stuck in a mental loop of worries and problems that seem to have no end? You’re probably ruminating, which is often a symptom of stress and anxiety. Here’s how to tell if your thought patterns have transitioned from regular overthinking into rumination, and how to stop them if they have, writes Hannah Seo of the New York Times.
Google’s head of mental health and wellbeing was among the 12,000 workers laid off by the company on Jan. 20. Kristin Maczko, who started working at Google in 2008, wrote in a LinkedIn post that “many people” on Google’s mental health and wellbeing team were let go.
Group Therapy is for informational purposes only and is not a substitute for professional mental health advice, diagnosis or treatment. We encourage you to seek the advice of a mental health professional or other qualified health provider with any questions or concerns you may have about your mental health.
Get Group Therapy
Life is stressful. Our weekly mental wellness newsletter can help.
You may occasionally receive promotional content from the Los Angeles Times.